Diabetes
Implantable ‘artificial pancreas’ could help diabetes patients control their blood sugar

|
Living with Type 1 diabetes requires constant monitoring of blood sugar levels and injecting insulin daily. Now scientists are reporting in the ACS journal Industrial & Engineering Chemistry Research the development of an implantable “artificial pancreas” that continuously measures a person’s blood sugar, or glucose, level and can automatically release insulin as needed.
Type 1 diabetes, previously known as juvenile diabetes, affects about 1.25 million Americans. About 200,000 of them are under 20 years old. The condition arises when a person’s own immune system destroys the pancreas cells that make insulin, the hormone that converts blood sugar into energy. To make up for this loss of insulin production, patients must take insulin daily. Current delivery methods involve multiple daily injections or insulin pump therapy, both requiring the user to actively track glucose and calculate the needed insulin dose. There is also a significant time lag between when a dose is needed and when it can take effect. Francis J. Doyle III and colleagues wanted to find a way to make monitoring and insulin delivery automatic and needle-free.
The researchers designed an algorithm that monitors blood sugar levels and computes an insulin dose that it delivers quickly and automatically when necessary.
Joslin researchers find drugs are effective for diabetic macular edema in new trial
|
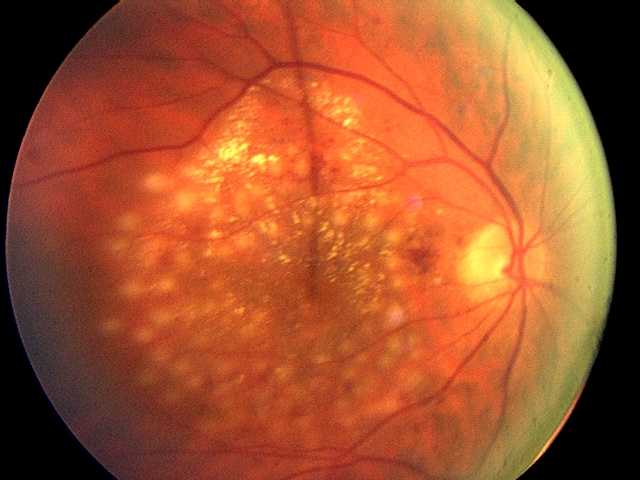
In the first clinical trial directly comparing three drugs most commonly used to treat diabetic macular edema, researchers found all were effective in improving vision and preventing vision loss. However, one drug, aflibercept, provided greater improvement for people with more severe vision loss when treatment was initiated. The trial was conducted by the National Eye Institute Diabetic Retinopathy Clinical Research Network (DRCR.net) including researchers from Joslin Diabetes Center. The results appeared in the February online edition of the New England Journal of Medicine.
Diabetes is a significant risk factor for developing eye diseases. The most common diabetic eye disease and a leading cause of blindness is diabetic retinopathy, which is caused by elevated blood sugar levels damaging the blood vessels of the retina and affects approximately 7.7 million Americans. About 750,000 Americans with diabetic retinopathy have diabetic macular edema (DME) in which fluid leaks into the macula, the area of the retina used when looking straight ahead. The fluid causes the macula to swell, blurring vision. “DME is the leading cause of moderate vision loss in working-age adults with diabetes. With the rate of diabetes increasing dramatically worldwide, many individuals will be at risk for vision loss from diabetic eye complications and DME is a major global health concern,” says Jennifer K. Sun, M.D., M.P.H., a member of the study research team and writing committee, and an Investigator in the Section on Vascular Biology, an ophthalmologist in Beetham Eye Institute at Joslin and an Assistant Professor at Harvard Medical School.
In an earlier study, Joslin researchers reported that VEGF, a major growth factor for blood vessels, is elevated in the eye fluids of patients with proliferative diabetic retinopathy and DME, causing leakage and the growth of abnormal blood vessels.
New superfoods could help key protein keep bodies healthy
|
|
A new generation of new superfoods that tackle heart disease and diabetes could be developed following research into a protein that helps keep cells in our bodies healthy.
Researchers at the University of Warwick found that the protein, called Nrf2, continually moves in and out of the nuclei of human cells to sense the cell’s health and vitality.
When Nrf2 is exposed to threats to the cell’s health it oscillates faster and activates an increase in the cell’s defence mechanism, including raising the levels of antioxidant.
The researchers, from the University’s Warwick Medical School, successfully increased the speed of Nrf2’s movement by artificially introducing health beneficial substances – potential components of new superfoods.
Poor quality of life may affect teens’ diabetes management
|
In the years after being diagnosed with diabetes, adolescents struggling with social and psychological burdens of managing the disease are likely to do a worse job of controlling it, according to a new U.S. study.
Teens who reported a lower quality of life were more likely to have rising levels of hemoglobin A1c, a marker of elevated blood sugar over time and a sign of poor diabetes control.
“We need to intervene from a prevention standpoint,” said Korey Hood, a psychologist at the University of California, San Francisco and lead author of the study. “We need to do systematic screening of these psychosocial issues.”
Teens who are psychologically stressed are less likely to take care of themselves, which could explain the rise in A1c levels, added Michael Scharf, a psychiatrist at the University of Rochester Medical Center who was not involved in the study.
Cancer drug protects against diabetes

|
New research shows that low doses of a cancer drug protect against the development of type 1 diabetes in mice. At the same time, the medicine protects the insulin-producing cells from being destroyed. The study is headed by researchers from the Faculty of Health and Medical Sciences at the University of Copenhagen, and has just been published in the distinguished scientific journal Proceedings of the National Academy of Sciences of the United States of America (PNAS).
Very low doses of a drug used to treat certain types of cancer protect the insulin-producing cells in the pancreas and prevent the development of diabetes mellitus type 1 in mice. The medicine works by lowering the level of so-called sterile inflammation. The findings have been made by researchers from the University of Copenhagen, the Technical University of Denmark and the University of Southern Denmark working with researchers in Belgium, Italy, Canada, Netherlands and the USA.
“Diabetes is a growing problem worldwide. Our research shows that very low doses of anticancer drugs used to treat lymphoma - so-called lysine deacetylase inhibitors - can reset the immune response to not attack the insulin-producing cells. We find fewer immune cells in the pancreas, and more insulin is produced when we give the medicine in the drinking water to mice that would otherwise develop type 1 diabetes,” says postdoc Dan Ploug Christensen, who is the first author on the article and responsible for the part of the experimental work carried out in Professor Thomas Mandrup-Poulsen’s laboratory at the Department of Biomedical Sciences, University of Copenhagen.
Amino acid’s increase is suspected in diabetes

|
Elevated levels of an amino acid, tyrosine, alter development and longevity in animals and may contribute to the development of diabetes in people, new research from the UT Health Science Center at San Antonio indicates. This line of study could potentially lead to a novel way to prevent or treat the disease. The research is reported this week [Dec. 19] in PLOS Genetics, a journal of the Public Library of Science.
Evidence of a direct effect in diabetes
Tyrosine is increased in the blood of people who are obese or diabetic, said study senior author Alfred Fisher, M.D., Ph.D., of the Barshop Institute for Longevity and Aging Studies at the UT Health Science Center. Among people who are obese, those at the highest risk of developing diabetes tend to have higher tyrosine levels. “It was unknown whether this was simply a marker of diabetes risk or could be playing a direct role in the disease,” Dr. Fisher said. “Our work suggests that tyrosine has a direct effect.”
Dr. Fisher is a physician scientist with the Barshop Institute’s Center for Healthy Aging and the Geriatric Research, Education and Clinical Center of the South Texas Veterans Health Care System. He has studied tyrosine’s effect on insulin signaling in an animal model called C. elegans (roundworms) since 2005. The observation that tyrosine was elevated in human diabetics further spurred the research. Now he is ready to take research insights back into people.
New Type 2 Diabetes Drug Onglyza Approved
.jpg)
|
The FDA today approved Onglyza, a once-daily treatment for type 2 diabetes to be taken in combination with diet and exercise.
Onglyza, made by Bristol-Myers Squibb and distributed by Bristol-Myers Squibb and AstraZeneca Pharmaceuticals, was tested in diabetes patients at relatively low risk of heart disease. The FDA approval requires Bristol-Myers Squibb to conduct a postmarketing study to evaluate the drug’s heart safety in higher-risk patients.
Onglyza carries the generic name saxagliptin. It belongs to a class of type 2 diabetes drugs called DPP-4 inhibitors. The first drug in this class, Merck’s Januvia, was approved in 2006. Like Onglyza, Januvia is taken once daily and is to be used in combination with diet and exercise.
Another DPP-4 inhibitor, Takeda’s alogliptin, was rejected by the FDA last month. The U.S. regulatory agency said the company has to provide more data on heart risks before it can be approved. Takeda has said these additional studies will take two years.
Mail order pharmacy use safe for people with diabetes

|
Most people with diabetes can safely get their medications though mail order pharmacies, a new study suggests.
Among some patients, getting drugs through the mail instead of in person was tied to a lower risk of ending up in the emergency department (ED), researchers found.
Mail order pharmacies are convenient, especially for people with disabilities or who can’t get to the pharmacy to pick up their regular orders, researchers said. But there have been concerns about those systems as well - for instance that people might miss out on important information by not seeing a pharmacist face-to-face.
“Mail order pharmacy use is actually fairly common in the United States and has become more and more so over the past 10 or 15 years,” Julie Schmittdiel told Reuters Health.
Policy considerations pose options for leaders to reduce costly disparities in diabetes
|
|
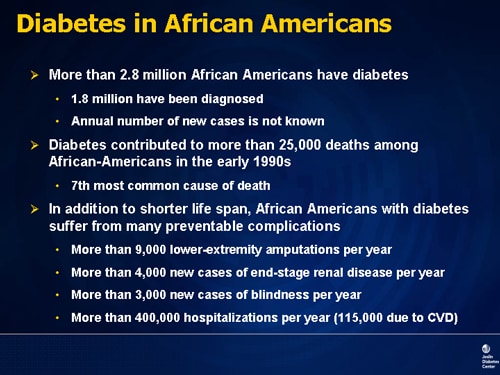
As newly elected or reelected national leaders consider paths forward for continued implementation of the Affordable Care Act, an innovative, locally-implemented program focused on reducing disparities in diabetes is releasing a new set of policy considerations to help inform decisions on national health policy.
The Alliance to Reduce Disparities in Diabetes, a national program launched and supported by The Merck Company Foundation, released “Policy Considerations That Make the Link,” that offers policymakers options for ways to advance changes to overcome the systemic and structural barriers that have blocked the ability to deliver and sustain effective diabetes care to those most in need.
“The document connects the on-the-ground experiences of the Alliance grantees with the issues facing national decision makers as they consider ways to get more value, quality, efficiency and innovation into our health care system,” Noreen Clark, PhD, Director of the Alliance’s National Program Office said.
The considerations pose a series of questions surrounding the identified need to realign financial incentives affecting health systems, providers and patients as a mechanism for reducing disparities in diabetes.
Cedars-Sinai study sheds light on bone marrow stem cell therapy for pancreatic recovery
|
|
Researchers at Cedars-Sinai’s Maxine Dunitz Neurosurgical Institute have found that a blood vessel-building gene boosts the ability of human bone marrow stem cells to sustain pancreatic recovery in a laboratory mouse model of insulin-dependent diabetes.
The findings, published in a PLOS ONE article of the Public Library of Science, offer new insights on mechanisms involved in regeneration of insulin-producing cells and provide new evidence that a diabetic’s own bone marrow one day may be a source of treatment.
Scientists began studying bone marrow-derived stem cells for pancreatic regeneration a decade ago. Recent studies involving several pancreas-related genes and delivery methods – transplantation into the organ or injection into the blood – have shown that bone marrow stem cell therapy could reverse or improve diabetes in some laboratory mice. But little has been known about how stem cells affect beta cells – pancreas cells that produce insulin – or how scientists could promote sustained beta cell renewal and insulin production.
Obesity-Linked Diabetes in Children Resists Treatment
|
|
Obesity and the form of diabetes linked to it are taking an even worse toll on America’s youths than medical experts had realized. As obesity rates in children have climbed, so has the incidence of Type 2 diabetes, and a new study adds another worry: the disease progresses more rapidly in children than in adults and is harder to treat.
“It’s frightening how severe this metabolic disease is in children,” said Dr. David M. Nathan, an author of the study and director of the diabetes center at Massachusetts General Hospital. “It’s really got a hold on them, and it’s hard to turn around.”
Before the 1990s, this form of diabetes was hardly ever seen in children. It is still uncommon, but experts say any increase in such a serious disease is troubling. There were about 3,600 new cases a year from 2002 to 2005, the latest years for which data is available.
Diabetes again linked to colon cancer risk
|
|
A new research review confirms that people with diabetes have a somewhat increased risk of colon cancer—but the reasons for the connection, and what should be done about it, remain unclear.
Combining the results of 14 international studies, researchers found that overall, people with diabetes were 38 percent more likely to be diagnosed with colon cancer than those who were diabetes-free.
There was also a 20 percent increase in the risk of rectal cancer, though that appeared to be confined to men.
Stem Cell “Memory” Can Boost Insulin Levels
|
|
Stem cells from early embryos can be coaxed into becoming a diverse array of specialized cells to revive and repair different areas of the body. Therapies based on these stem cells have long been contemplated for the treatment of diabetes, but have been held back by medical and ethical drawbacks.
Now researchers at Tel Aviv University are capitalizing on the “memories” of stem cells generated from adult cells to bring new hope to sufferers of juvenile or type 1 diabetes, which affects three million people in the United States.
Prof. Shimon Efrat of TAU’s Department of Human Molecular Genetics and Biochemistry at the Sackler Faculty of Medicine, says these “induced pluripotent stem cells,” derived from adult cells, represent an embryonic-like state. To some degree, he found, the cells retain a “memory” of what they once were — when created from pancreatic beta cells, the cells responsible for the production of insulin, these pluripotent cells prove more efficient than their embryonic counterparts in creating insulin-producing cells. Prof. Efrat says that this discovery promises to advance the development of cell replacement therapy for diabetics, possibly leading to an effective alternative to organ transplants.
Johns Hopkins scientists link DNA ‘end-caps’ length to diabetes risk
|
|
New evidence has emerged from studies in mice that short telomeres or “caps” at the ends of chromosomes may predispose people to age-related diabetes, according to Johns Hopkins scientists.
Telomeres are repetitive sequences of DNA that protect the ends of chromosomes, and they normally shorten with age, much like the caps that protect the end of shoelaces. As telomeres shorten, cells lose the ability to divide normally and eventually die. Telomere shortening has been linked to cancer, lung disease, and other age-related illnesses. Diabetes, also a disease of aging, affects as many as one in four adults over the age of 60.
The Johns Hopkins research, described in the March 10 issue of PLoS One, arose from scientist Mary Armanios’ observation that diabetes seems to occur more often in patients with dyskeratosis congenita, a rare, inherited disease caused by short telomeres. Patients with dyskeratosis congenita often have premature hair graying and are prone to develop early organ failure.
CHEO opens new “active living” clinic for children to fight diabetes
|
|
Severely obese children and those at high risk of type 2 diabetes will have a place to get counselling and treatment with the opening of a new outpatient clinic run by the Children’s Hospital of Eastern Ontario.
Among other things, the Centre for Healthy Active Living will provide early screening to children who have at least one parent with type 2 diabetes, commonly linked to sedentary lifestyles and diets loaded with fat and sugar. Research suggests children of parents with type 2 diabetes have a higher risk of developing the disease themselves.
Diabetes, which disrupts sugar uptake in the blood, is the leading cause of blindness, amputations and kidney failure; over a lifetime, it can triple a person’s risk for heart attack, stroke and Alzheimer’s disease.





