Gene may open door for improved keloid, scar treatment
|
Researchers at Henry Ford Hospital in Detroit have identified a gene that may offer a better understanding of how keloid scars develop and potentially open the door to improved treatment for the often painful, itchy and tender scars.
The study is the first to demonstrate that an altered AHNAK gene may have a significant biological role in keloid development.
“This finding has great promise for better understanding how keloids function and offer a potential target for improved and novel treatments,” says study lead author Lamont R. Jones, M.D., Vice Chair, Department of Otolaryngology-Head and Neck Surgery at Henry Ford.
“We now have a better understanding of how this gene fits in the broader picture of the wound healing process, which may be important in preventing scars in general.”
Study results will be presented today, Jan. 23, at the 2015 Triological Combined Sections Meeting in San Diego.
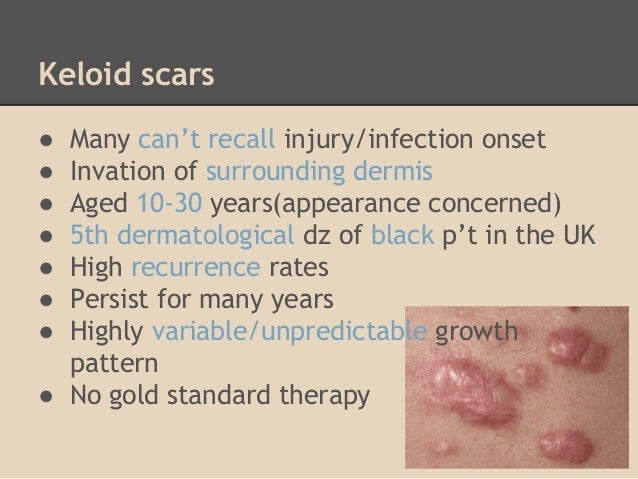
Keloid scars form raised, firm skin areas and most often occur on the chest, shoulders, earlobes (following ear piercing), upper arms and cheeks. Unlike regular scars, keloids do not subside over time and often extend outside the wound site.
The lowest rates of keloid formation have been documented in albinos and the highest seen in dark skinned individuals, especially in the African-American population.
When skin is injured, fibrous tissue (called scar tissue) forms over the wound to repair and protect the injury. In some cases, scar tissue grows excessively, forming smooth, hard growths called keloids. Keloids can be much larger than the original wound, and are most commonly found on the upper chest and shoulders. However, keloids can affect any part of the body. (NZDSI)
Although keloids are not harmful to your health, they may present cosmetic concerns.
What Symptoms Are Associated with Keloids?
Keloids occur from the overgrowth of scar tissue; symptoms will occur at a site of previous skin injury.
Symptoms include:
area that is flesh-colored, pink or red in color
a lumpy or ridged area of skin
an area that continues to grow larger with scar tissue over time
itchy patch of skin
Keloid scars tend to be larger than the original wound itself. They may take weeks or months to fully develop.
While keloid scars may be itchy, they are typically not harmful to your health. You may experience some discomfort or tenderness, or possible irritation from clothing or other forms of friction. In rare instances, a person may experience keloid scarring on a significant amount of their body. When this occurs, the hardened, tight scar tissue may restrict your movements.
Keloids are often more of a cosmetic concern than a health one. You may feel self-conscious if the keloid is very large or in a highly visible location, such as an earlobe or on the face. Sun exposure or tanning may discolor the scar tissue, making it slightly darker than your surrounding skin. This can make the keloid stand out even more than it already does. Keep the scar covered when you are in the sun to prevent discoloration.
Treatment for keloids includes cortisone injections, pressure dressings, silicone gels, surgery, cryosurgery (freezing), laser treatment, or radiation therapy. A combination of treatments may be used, depending on the individual. In some cases, keloids return after treatment, up to 50 to 100 percent of the time.
AHNAK is a 700 kDa protein located on the cell membrane in epithelial cells and in the nucleus and cytoplasm of other cell types such as fibroblasts. AHNAK has been suspected to contribute to cell-cell adhesion or exocytosis.
 For their study, Dr. Jones and his colleges investigated AHNAK as a potential biomarker in keloids through the integration of methylation and gene expression.
For their study, Dr. Jones and his colleges investigated AHNAK as a potential biomarker in keloids through the integration of methylation and gene expression.
To do so, the Henry Ford team examined samples of fresh keloid tissue and fresh normal tissue for AHNAK expression.
Three of the five keloid samples showed a large reduction in expression as compared to the normal tissue.
What are keloid scars?
Collagen gathers around the damage and builds up to help the wound seal over. The resulting scar usually fades over time, becoming smoother and less noticeable.
However, some scars don’t stop growing. They “invade” the surrounding healthy skin and become bigger than the original wound. These are known as keloid scars.
Some scars become red and raised within the size of the original wound. These are called hypertrophic scars. Find out more about hypertrophic scars.
“A keloid scar is an overgrown scar that can spread outside the original area of skin damage,” says Hermione Lawson of the British Skin Foundation. “Keloid scars are shiny and hairless, they’re raised above the surrounding skin, and can feel hard and rubbery.”
Keloids affect around 10-15% of all wounds. They can appear anywhere on the body, but usually form on the shoulders, head and neck.
They can last for years and sometimes don’t form until months or years after the initial injury. New keloid scars are sometimes red or purple. They’re not usually painful, but some people feel embarrassed or upset if they think the scar is disfiguring them.
Experts don’t fully understand why keloid scarring happens, but these scars are not contagious (they’re not catching) and there is no risk of them turning into cancer.
In this small sample, gene expression was consistent with methylation, a process that allows the researchers to look for genetic abnormalities within tumor samples.
“Identifying AHNAK puts our translational research one step closer to moving from the bench to the bedside,” says Dr. Jones.
###
In addition to Dr. Jones, study co-authors from Henry Ford are Joshua Greene, M.D.; Kang Mei Chen, M.D.; George Divine, Ph.D.; Dhananjay Chitale, M.D.; Veena Shah, M.D.; and Maria J. Worsham, Ph.D.
###
Krista Hopson Boyer
.(JavaScript must be enabled to view this email address)
313-874-7207
Henry Ford Health System
Print Version
Tell-a-Friend comments powered by Disqus





