New biomarkers may influence drug design and alternative treatments of cancer, study shows

|
Researchers have discovered gene-targets (biomarkers) that may enable alternative treatments or the potential design of new drugs that target metastasis-promoting tumor genes.
This is the key finding in a study led by researchers from Georgia State University in collaboration with the University of Oklahoma College of Medicine and published in journal Oncotarget.
The spread of cancer cells from the initial site of occurrence (primary site) to other secondary tissues is called metastasis, and contributes to poor or limited response of cancer cells to treatments, which results in death. For example, cancer cells initially in the lungs can begin to spread to other organs, including the brain and liver.
Gynecologic cancer typically originates from the female reproductive organs, and include endometrial and ovarian cancer, among others. Survival rates are typically very poor for these cancer-types, with limited response to existing therapies. A major reason for poor survival rates is late diagnoses, by which time the cancer cells have spread to secondary sites.
“The aim of our study was to investigate/search for gene targets that provide meaningful information on the tendency of cancer cells to spread to secondary sites,” said Imoh Okon, assistant professor of research in the Center for Molecular and Translational Medicine at Georgia State and lead author on the study. “In this study, we found that enhanced neuropilin-1 (NRP-1) and NEDD9 levels in endometrial and lung cancer positively correlated with metastasis, while liver kinase B1 (LKB1) inhibited the migration of cancer cells.”
For the study, researchers obtained more than a hundred clinical endometrial cancer specimens and matching serum. Using multiplex arrays and a variety of experimental approaches, they analyzed the specimens for gene targets that positively or negatively correlated with metastatic potential of the tumors. Data were translated to reflect the patient’s age at diagnosis, disease stage, grade and histology.
“Our research provides strong translational potential with respect to biomarkers that play critical roles in the development of endometrial/lung tumors,” added Okon. “The ability to identify, characterize and validate gene targets that strongly associate or correlate with disease development or metastasis will facilitate early detection and appropriate treatments to tackle the disease at an early stage or before metastasis occurs.”
The researchers’ next steps will involve expansion of the biomarkers identified in this study to other cancer types, especially breast cancer, due to the hormonal input that is a common factor in gynecologic tumors.
Confirmation of the biomarkers in other cancer types will facilitate further characterization and validation to provide mechanistic understanding of how and why these specific gene-targets become modulated to accentuate or inhibit tumor metastasis. The overall goal will be to test potential biomarker function or development of new drugs that target the identified genes.
###
Brian Mullen
.(JavaScript must be enabled to view this email address)
404-413-5464
Georgia State University
UGA ecologist finds another cause of antibiotic resistance

|
While the rapid emergence of antibiotic-resistant bacteria has prompted the medical community, non-profit organizations, public health officials and the national media to educate the public to the dangers of misusing and overusing antibiotics, the University of Georgia’s J. Vaun McArthur is concerned that there’s more to the problem than the misuse of common medications.
McArthur, a senior research ecologist with the Savannah River Ecology Laboratory and Odum School of Ecology, believes environmental contaminants may be partly to blame for the rise in bacterial resistance, and he tested this hypothesis in streams on the U.S. Department of Energy’s Savannah River Site.
The 310-square mile site near Aiken, South Carolina, east of the Savannah River, was closed to the public in the early 1950s to produce materials used in nuclear weapons. This production led to legacy waste, or contamination, in limited areas of the site. This waste impacted some of the streams in the industrial areas.
“The site was constructed and closed to the public before antibiotics were used in medical practices and agriculture,” McArthur said. “The streams have not had inputs from wastewater, so we know the observed patterns are from something other than antibiotics.”
McArthur tested five antibiotics on 427 strains of E. coli bacteria in the streams. His research team collected samples from 11 locations in nine streams, which included sediment as well as water samples. The level of metal contamination among these locations varied from little to high.
The results, published in the journal Environmental Microbiology, revealed high levels of antibiotic resistance in eight of the 11 water samples. The highest levels were found at the northern location of Upper Three Runs Creek, where the stream system enters the site, and on two tributaries located in the industrial area, U4 and U8. The level of antibiotic resistance was high in both water and sediment samples from these streams.
McArthur said Upper Three Runs Creek flows through residential, agricultural and industrial areas before it enters the SRS, so the bacteria in this stream have been exposed to antibiotics. In contrast, U4 and U8 are completely contained within the site and have no known input from antibiotics. However, they have a long history of inputs from the legacy waste.
McArthur conducted a second screening using 23 antibiotics on U4, U8 and U10, a nearby stream with little to no industrial impact.
“More than 95 percent of the bacteria samples from these streams were resistant to 10 or more of the 23 antibiotics,” McArthur said. These included front-line antibiotics—gatifloxacin and ciprofloxacin, which are used to treat basic bacterial infections from pink eye to urinary tract and sinus infections.
The contaminated streams U4 and U8 had the highest level of antibiotic resistance.
“These streams have no source of antibiotic input, thus the only explanation for the high level of antibiotic resistance is the environmental contaminants in these streams—the metals, including cadmium and mercury,” McArthur said.
McArthur said the three tributaries of Upper Three Runs Creek, U4, U8 and U10 vary in the level of contamination respectively, from highly impacted and impacted to not as impacted.
It is possible that antibiotic-exposed wildlife may have dumped waste into these streams, MacArthur said, but only streams with a history of industrial input had antibiotic-resistant bacteria. Bacteria in the six streams in the pristine areas of the site were susceptible to the antibiotics.
McArthur said it is concerning that these antibiotic-resistant streams drain into the Savannah River, a large body of water bordering Georgia and South Carolina. The Savannah River shares at least two major characteristics with many large bodies of water in the U.S. It is in close proximity to residential communities, and it receives industrially contaminated water—prone to antibiotic resistance.
“The findings of this study may very well explain why resistant bacteria are so widely distributed,” McArthur said.
###
Additional researchers on this study include R. Cary Tuckfield, Ecostatys, LLC, Aiken, S.C.; Craig Baker-Austin, Centre for Environment, Fisheries and Aquaculture Science, Lowestoft, U.K.; and Dean E. Fletcher, UGA Savannah River Ecology Laboratory, Aiken, S.C.
The study, ‘Patterns of Multi-Antibiotic-Resistant Escherichia Coli from Streams with No History of Antimicrobial Inputs,’ is available at http://link.springer.com/article/10.1007/s00248-015-0678-4/fulltext.html.
###
Stephanie Schupska
[email protected]
706-542-6927
Don’t Blame Breast Density; $$$ Toxicity; ‘Nurse Ratched’ Returns
|
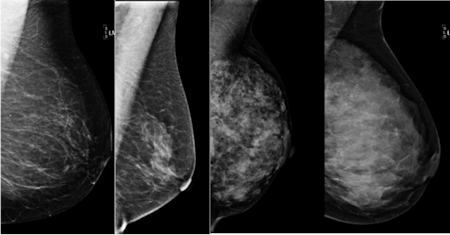
Age and body weight, not breast-tissue density, drive a woman’s risk of breast cancer, according to a study from Johns Hopkins.
An 8-year-old Utah girl has developed only the 35th known case of secretory breast carcinoma, a rare form of breast cancer that occurs in young girls.
The “financial toxicity” of cancer is not unique to the U.S., as an American oncologist learned over dinner with two colleagues practicing in the nation of Georgia.
Two pediatric oncologists share their insights into to dealing with the “unsung heartache” of caring for children with cancer.
Although the clinical decision-making process has become infinitely more complex, computer algorithms and other high-tech aids still can’t replace clinician judgment for helping cancer patients maneuver through some of the most difficult choices.
The survival odds for stage IV breast cancer remain poor but still improve significantly with surgery, authors of a new study concluded in JAMA Surgery.
After a series of regulatory wins, Bristol-Myers Squibb’s immune checkpoint inhibitor nivolumab (Opdivo) failed to gain FDA approval for treatment of BRAF-positive metastatic melanoma, according to Seeking Alpha.
A rock singer and a filmmaker collaborate in a unique way to make the point that men develop breast cancer, too, Forbes reports.
Women with breast cancer had significantly better progression-free survival if they participated in organized stress-reduction activities beginning soon after diagnosis, according to Newsmax.
The government of Haiti, with financial assistance from Boston-based Partners in Health, has implemented a large-scale screening program for cervical cancer and vaccination of girls against human papillomavirus infection in an effort to reverse the country’s high incidence of the cancer and associated mortality, as reported by Associated Press.
A caring husband talks about being “Nurse Ratched” to help his wife deal with cancer-related pain.
###
(Fox News)
Metabolic profiles distinguish early stage ovarian cancer with unprecedented accuracy

|
Studying blood serum compounds of different molecular weights has led scientists to a set of biomarkers that may enable development of a highly accurate screening test for early-stage ovarian cancer.
Using advanced liquid chromatography and mass spectrometry techniques coupled with machine learning computer algorithms, researchers have identified 16 metabolite compounds that provided unprecedented accuracy in distinguishing 46 women with early-stage ovarian cancer from a control group of 49 women who did not have the disease. Blood samples for the study were collected from a broad geographic area - Canada, Philadelphia and Atlanta.
While the set of biomarkers reported in this study are the most accurate reported thus far for early-stage ovarian cancer, more extensive testing across a larger population will be needed to determine if the high diagnostic accuracy will be maintained across a larger group of women representing a diversity of ethnic and racial groups.
The research is scheduled to be reported November 17 in the journal Scientific Reports, an open access journal from the publishers of Nature.
“This work provides a proof of concept that using an integrated approach combining analytical chemistry and learning algorithms may be a way to identify optimal diagnostic features,” said John McDonald, a professor in the School of Biology at the Georgia Institute of Technology and director of its Integrated Cancer Research Center. “We think our results show great promise and we plan to further validate our findings across much larger samples.”
Ovarian cancer has been difficult to treat because it typically is not diagnosed until after it has metastasized to other areas of the body. Researchers have been seeking a routine screening test that could diagnose the disease in stage one or stage two - when the cancer is confined to the ovaries.
Working with three cancer treatment centers in the U.S. and Canada, the Georgia Tech researchers obtained blood samples from women with stage one and stage two ovarian cancer. They separated out the serum, which contains proteins and metabolites - molecules produced by enzymatic reactions in the body.
The serum samples were analyzed by ultra-performance liquid chromatography-mass spectrometry (UPLC-MS), which is two instruments joined together to better separate samples into their individual components. Heavier molecules are separated from lighter molecules, and the molecular signatures are determined with enough accuracy to identify the specific compounds. The Georgia Tech researchers decided to look only at the metabolites in their research.
“People have been looking at proteins for diagnosis of ovarian cancer for a couple of decades, and the results have not been very impressive,” said Facundo Fernández, a professor in Georgia Tech’s School of Chemistry and Biochemistry who led the analytical chemistry part of the research. “We decided to look in a different place for molecules that could potentially provide diagnostic capabilities. It’s one of the places that people had really not studied before.”
Samples from each of the 46 cancer patients were divided so they could be analyzed in duplicate. The researchers also looked at serum samples from 49 women who did not have cancer. The work required eliminating unrelated compounds such as caffeine, and molecules that were not present in all the cancer patients.
“We used really high resolution equipment and instrumentation to be able to separate most of the components of the samples,” Fernández explained. “Otherwise, detection of early-stage ovarian cancer is very difficult because you have a lot of confounding factors.”
The chemical work identified about a thousand candidate compounds. That number was reduced to about 255 through the work of research scientist David Gaul, who removed duplicates and unrelated molecules from the collection.
These 255 compounds were then analyzed by a learning algorithm which evaluated the predictive value of each one. Molecules that did not contribute to the predictive accuracy of the screening were eliminated. Ultimately, the algorithm produced a list of 16 molecules that together differentiated cancer patients with extremely high accuracy - greater than 90 percent.
“The algorithm looks at the metabolic features and correlates them with whether the samples were from cancer or control patients,” McDonald explained. “The algorithm has no idea what these compounds are. It is simply looking for the combination of molecules that provides the optimal predictive accuracy. What is encouraging is that many of the diagnostic features identified are metabolites that have been previously implicated in ovarian cancer.”
As a next step, McDonald and Fernández would like to study samples from a larger population that includes significant numbers of different ethnic and racial groups. Those individuals may have different metabolites that could serve as biomarkers for ovarian cancer.
Though sophisticated laboratory equipment was required to identify the 16 molecules, a screening test would not require the same level of sophistication, Fernández said.
“Once you know what these molecules are, the next step would be to set up a clinical assay,” he said. “Mass spectrometry is a common tool in this field. We could use a clinical mass spectrometer to look at only the molecules we are interested in. Moving this to a clinical assay would take work, but I don’t see any technical barriers to doing it.”
The Fernández and McDonald groups have used a similar approach with prostate cancer and plan to explore its utility for detecting other types of cancer.
###
The research was supported by grants from The Laura Crandall Brown Ovarian Cancer Foundation, The Ovarian Cancer Research Fund, The Ovarian Cancer Institute, Northside Hospital (Atlanta), The Robinson Family Fund, and the Deborah Nash Endowment Fund.
CITATION: David A. Gaul, et al., “Highly-accurate metabolomics detection of early-stage ovarian cancer,” (Scientific Reports, 2015).
###
John Toon
[email protected]
404-894-6986
GEORGIA INSTITUTE OF TECHNOLOGY
Moffitt researchers develop first genetic test to predict tumor sensitivity to radiation therapy

|
Recent advances in the understanding of cancer have led to more personalized therapies, such as drugs that target particular proteins and tests that analyze gene expression patterns in tumors to predict a patient’s response to therapy. Moffitt Cancer Center researchers have contributed to these advances by developing the first test that analyzes the sensitivity of tumors to radiation therapy. They discovered that colon cancer metastases have varying sensitivity to radiation therapy based on their anatomic location.
Researchers from Moffitt previously developed a radiation sensitivity index (RSI) that predicts how sensitive tumors are to radiation based on expression patterns of different genes. In a paper published July 15 in The International Journal of Radiation Oncology, Biology and Physics, they used the RSI to determine the radiation sensitivity of 704 metastatic and 1362 primary colon tumors.
They discovered that metastatic colon tumors are more resistant to radiation than primary colon tumors. The researchers also report that radiation sensitivity may be dependent on the anatomic location of the tumor metastasis. This is one of the first research studies to highlight the importance of the location of the metastasis as well as the location of the original primary tumor, in predicting response to radiation therapy. The researchers confirmed some of these findings by analyzing how effective radiation therapy was in 29 colon cancer tumors that metastasized to either the liver or lung. Their findings validated that those patients who had metastatic disease in their lungs had a better response to radiation then patients who had metastatic disease in their liver, as predicted by RSI.
This study suggests that it may be possible to personalize radiation therapy for patients. “Radiation sensitivity index provides the first opportunity to use tumor genetics to guide and optimize the radiation dose that patients receive. The consequences for this can be quite dramatic. We have estimated that up to 15 percent of patients will be candidates for dose optimization,” explained senior study author Javier F.Torres-Roca, MD, director of Clinical Research and associate member of the Department of Radiation Oncology at Moffitt.
The medical community has noted Moffitt’s contributions to improving cancer care. According to editors of the International Journal of Radiation Oncology, Biology and Physics who highlighted the study in a commentary, “Radiation sensitivity index is important progress towards personalizing radiation therapy. The results generate important hypotheses that could dramatically influence patient care.”
###
The research was made possible through patient samples acquired through Moffitt’s Total Cancer Care® Program. Total Cancer Care is a partnership between patients, physicians and researchers. Cancer patients who consent to be a part of the program donate tissue and blood specimens and provide background information to enable physicians and researchers to study cancer development, prevention and treatment. The acquisition of large amounts of data through the Total Cancer Care Program may lead to better cancer therapies that are personalized to each patient.
The research was supported by grants and awards received from the National Institutes of Health (R21CA101355 and R21CA135620), the US Army Medical Research and Materiel Command, the National Functional Genomics Center (170220051), the Bankhead-Coley Foundation (09BB-22), and the DeBartolo Family Personalized Medicine Institute.
About Moffitt Cancer Center
Located in Tampa, Moffitt is one of only 41 National Cancer Institute-designated Comprehensive Cancer Centers, a distinction that recognizes Moffitt’s excellence in research, its contributions to clinical trials, prevention and cancer control. Moffitt is the top-ranked cancer hospital in the Florida and has been listed in U.S. News & World Report as one of the “Best Hospitals” for cancer care since 1999. With more than 4,500 employees, Moffitt has an economic impact in the state of nearly $1.6 billion. For more information, visit MOFFITT.org, and follow the Moffitt momentum on Facebook, Twitter and YouTube.
###
Kim Polacek
[email protected]
813-745-7408
Sex and violence may not really sell products

|
f there’s one thing advertisers think they know, it is that sex and violence sell.
A new analysis, however, provides some of the best evidence to date that this widely accepted adage just isn’t true.
Researchers analyzed the results of 53 different experiments (a so-called meta-analysis) involving nearly 8,500 people, done over 44 years. All of these experiments examined some facet of the question of whether sexual or violent media content could help sell advertised products.
When all the results are considered together, the overall conclusion, with some caveats, is that programs featuring violence and sex aren’t the ideal context for effective advertising, said Brad Bushman, co-author of the study and professor of communication and psychology at The Ohio State University.
It’s not that people don’t pay attention to sex and violence in the media, Bushman said. In fact, an evolutionary perspective would say it is just the opposite.
“People are so focused on the sex and violence they see in the media that they pay less attention to the advertising messages that appear along with it,” Bushman said.
“Advertisers shouldn’t be so sure that sex and violence can help them sell their products.”
 Bushman conducted the study with Robert Lull, who just earned his Ph.D. in communication at Ohio State. The results were published online yesterday in the journal Psychological Bulletin and will be featured in a future print edition.
Bushman conducted the study with Robert Lull, who just earned his Ph.D. in communication at Ohio State. The results were published online yesterday in the journal Psychological Bulletin and will be featured in a future print edition.
Their analysis included studies involving a variety of types of media, including print, TV, movies and even a few video games. They examined studies in which the ads themselves contained sex or violence and studies in which only the media surrounding the ads contained such content.
In all cases, the researchers had studied whether sex and violence affected brand memory, brand attitudes and people’s intention to buy the products advertised.
They found that memory for brands and ads was significantly impaired in programs containing sex, violence, or both sex and violence.
Overall, people had less favorable attitudes toward brands that advertised in violent media compared to neutral media. Only one study examined attitudes toward brands in sexual media and that pointed toward less favorable attitudes as well.
And people reported less intention to buy brands that were advertised in media containing violence, sex or both, compared to the same brands in media containing no sex or violence.
But what about ads that themselves featured sex and violence? Here, the findings were not as clear-cut. Overall, memory for brands that featured sex and violence was not impaired.
But attitudes toward brands that featured sexual ads were significantly lower than those same brands in neutral ads. Only one study examined attitudes toward brands in violent ads and those results also trended toward less favorable attitudes.
Overall, buying intentions did not depend on whether the ad contained sex or violence.
While these overall conclusions were clear, Lull and Bushman found several nuances in the studies they examined.
Memory for ads and buying intentions were both improved when the ad content and the media content were matching in terms of sex and violence. For example, violent ads worked best when they were paired with violent programs, Lull said.
“If a TV program prompts violent or sexual thoughts, an ad that prompts similar thoughts will be better remembered,” Lull said.
Sexual ads didn’t hurt brand attitudes and buying intentions overall. But the higher the levels of sexual content in the ads, the more negative the attitude people had toward the brand and the less likely they were to say they would buy the product.
Older people in the studies were less likely to say they would buy products featured in violent or sexual ads, compared to younger people.
Men’s brand memory was more impaired than women’s when watching media content or ads featuring sexual or violent imagery.
“This fits in with evolutionary theory that suggests males pay more attention to violence and sex than women do,” Lull said. “Because they’re paying more attention to this content, they are less likely to remember the ads.”
Another interesting finding was that memory impairments and negative attitudes toward brands featured in violent or sexual ads have actually decreased over the past decades.
This study can’t say for sure, but one explanation is that people have started to become desensitized to sex and violence in ads, Bushman said
“Viewers are so accustomed to seeing violent and sexual media content that they don’t respond as much today to the attention-grabbing impact as they did in previous decades,” he said.
Bushman said he is continuing work in his laboratory to examine the effects of violent ads on memory.
###
Contact: Brad Bushman, 614-688-8779; [email protected]
Robert Lull, [email protected]
Media contact: Pam Gorder, 614-292-9475; [email protected]
Anxiety increases the risk of gastrointestinal infection and long-term complications

|
A team comprised of scientists at VIB, KU Leuven and UZ Leuven has made significant progress in uncovering the connection between psychological factors and the immune system. Their findings are based on an investigation of a massive drinking water contamination incident in Belgium in 2010, and are now published in the leading international medical journal Gut.
In December 2010, the Belgian communities of Schelle and Hemiksem in the province of Antwerp faced an outbreak of gastroenteritis, with more than 18,000 people exposed to contaminated drinking water. During the outbreak, VIB and KU Leuven set up a scientific task force to study the incident’s long-term effects, led by Guy Boeckxstaens (UZ Leuven / KU Leuven) and Adrian Liston (VIB / KU Leuven).
Seizing an unexpected opportunity
Adrian Liston (VIB/KU Leuven): “The water contamination in Schelle and Hemiksem was an ‘accidental experiment’ on a scale rarely possible in medical research. By following the patients from the initial contamination to a year after the outbreak we were able to find out what factors altered the risk of long-term complications.”
Anxiety and depression affect immune system
The scientists found that individual with higher levels of anxiety or depression prior to the water contamination developed gastrointestinal infections of increased severity. The same individuals also had an increased risk of developing the long-term complication of irritable bowel syndrome, with intermittent abdominal cramps, diarrhea or constipation a year after the initial contamination.
Guy Boeckxstaens (UZ Leuven / KU Leuven): “Irritable Bowel Syndrome is a condition of chronic abdominal pain and altered bowel movements. This is a common condition with large socio-economic costs, yet there is so much that still remains to be discovered about the causes. Our investigation found that that anxiety or depression alters the immune response towards a gastrointestinal infection, which can result in more severe symptoms and the development of chronic irritable bowel syndrome.”
Psychological factors key in preventing long-term complications
The study’s results provide valuable new insight into the cause of irritable bowel syndrome, and underscoring the connection between psychological factors and the immune system.
Adrian Liston (VIB/KU Leuven): “These results once again emphasize the importance of mental health care and social support services. We need to understand that health, society and economics are not independent, and ignoring depression and anxiety results in higher long-term medical costs.”
###
Sooike Stoops
[email protected]
32-924-46611
VIB (the Flanders Institute for Biotechnology)
Implantable ‘artificial pancreas’ could help diabetes patients control their blood sugar

|
Living with Type 1 diabetes requires constant monitoring of blood sugar levels and injecting insulin daily. Now scientists are reporting in the ACS journal Industrial & Engineering Chemistry Research the development of an implantable “artificial pancreas” that continuously measures a person’s blood sugar, or glucose, level and can automatically release insulin as needed.
Type 1 diabetes, previously known as juvenile diabetes, affects about 1.25 million Americans. About 200,000 of them are under 20 years old. The condition arises when a person’s own immune system destroys the pancreas cells that make insulin, the hormone that converts blood sugar into energy. To make up for this loss of insulin production, patients must take insulin daily. Current delivery methods involve multiple daily injections or insulin pump therapy, both requiring the user to actively track glucose and calculate the needed insulin dose. There is also a significant time lag between when a dose is needed and when it can take effect. Francis J. Doyle III and colleagues wanted to find a way to make monitoring and insulin delivery automatic and needle-free.
The researchers designed an algorithm that monitors blood sugar levels and computes an insulin dose that it delivers quickly and automatically when necessary.
The algorithm is designed to work with implanted devices, specifically with an artificial pancreas, and would overcome the delays experienced with current devices. Computer testing of the algorithm simulated the rise and fall of glucose that would correspond to meals and an overnight period of sleep. The artificial pancreas maintained blood glucose within the target range nearly 80 percent of the time. The researchers say they will soon test the device in animals.
###
The authors acknowledge funding from the National Science Foundation and the National Institutes of Health.
The American Chemical Society is a nonprofit organization chartered by the U.S. Congress. With more than 158,000 members, ACS is the world’s largest scientific society and a global leader in providing access to chemistry-related research through its multiple databases, peer-reviewed journals and scientific conferences. Its main offices are in Washington, D.C., and Columbus, Ohio.
To automatically receive news releases from the American Chemical Society, contact [email protected].
###
Michael Bernstein
[email protected]
202-872-6042
American Chemical Society
New drug for neuroblastoma shows promise in phase I study

|
Researchers at Spectrum Health Helen DeVos Children’s Hospital have completed the first clinical trial of a new treatment for children suffering from neuroblastoma. In a clinical trial led by Giselle Sholler, MD, pediatric oncologist at Helen DeVos Children’s Hospital and the Neuroblastoma and Medulloblastoma Translational Research Consortium (NMTRC), DFMO, an investigational agent, showed minimal side effects with long-term survival of three patients. This is the first clinical study of an oral dosing form of DFMO in any pediatric population.
“This DFMO trial is an important advancement in neuroblastoma research,” explained Dr. Sholler. “We believe that by using DFMO to target an important cancer stem cell pathway to ‘turn cells off,’ we may prevent children from relapsing. Cancer cells have pathways that drive the cancer to grow and DFMO targets a specific pathway to turn these cells off.”
Dr. Sholler recently published her laboratory studies describing how this drug works in neuroblastoma in preventing tumor formation in lab models and also published the full results of the phase one trial.
Will Lacey, a patient in the phase 1 clinical trial, was free from side effects and needed no additional treatment following the trial. This is a new way of life for a 10-year old whose neuroblastoma had kept him in and out of hospitals and on various treatments for most of his life.
Patrick Lacey, Will’s father explained, “His quality-of-life has been amazing! He was never in the hospital and he was indistinguishable from his peers. Will has had an incredible two and a half years and has not required any further tumor directed therapy since.”
Key findings of the trial include:
DFMO is well tolerated with minimal side effects in children with relapsed neuroblastoma
Children with specific genetic changes are predicted to have better response to DFMO
There were three patients enrolled in the trial who are now long-term survivors
Dr. Sholler’s laboratory investigated the effectiveness of combining DFMO with the drug etoposide. She incorporated early work performed by Dr. Andre Bachmann, professor of pediatrics and human development at Michigan State University College of Human Medicine. Dr. Bachmann’s work identified the relationship of this drug targeting the ODC gene in neuroblastoma. Dr. Sholler then designed and led a clinical trial to test the combination of drugs in children being treated for the disease at sites participating in the NMTRC. Dr. Sholler and NMTRC are now testing this concept in a Phase II clinical trial to prevent relapse.
“Since 2001, I have focused my research career on translating DFMO from bench to clinic, and a dream has come true,” said Dr. Bachmann. “DFMO is now available to neuroblastoma patients thanks to Dr. Sholler and the wonderful NMTRC team.”
Dr. Sholler received her M.D. from New York Medical College, in Valhalla, NY. She was a resident in pediatrics and, subsequently, a fellow in pediatric hematology/oncology at Brown University, before coming to international prominence for her work with relapsed neuroblastoma at the University of Vermont. She then transferred her clinical program to Helen DeVos Children’s Hospital in Grand Rapids. She is now Haworth Endowed Director of the Innovative Therapeutics Clinic focused on early phase clinical trials for pediatric cancers and Department of Pediatrics. Here she sees patients as part of the NMTRC which she chairs. Dr. Sholler’s lab research at Helen DeVos Children’s Hospital where she runs the NMTRC Research Laboratory is focused on identifying new therapies for children with neuroblastoma.
###
About NMTRC
The Neuroblastoma and Medulloblastoma Translational Research Consortium (NMTRC) is a group of 24 universities and children’s hospitals headquartered at the Helen DeVos Children’s Hospital that offer a nationwide network of childhood cancer clinical trials. These trials are based on the research from a group of closely collaborating investigators who are linked with laboratory programs developing novel therapies for high-risk neuroblastoma and medulloblastoma.
About Spectrum Health
Spectrum Health is a not-for-profit health system, based in West Michigan, offering a full continuum of care through the Spectrum Health Hospital Group, which is comprised of 12 hospitals, including Helen DeVos Children’s Hospital; 180 ambulatory and service sites; 1,300 physicians and advanced practice providers, which include 1,100 members of the Spectrum Health Medical Group; and Priority Health, a health plan with more than 648,000 members. Spectrum Health is West Michigan’s largest employer, with 22,600 employees. The organization provided $294.6 million in community benefit during its 2014 fiscal year. Spectrum Health is the only health system in Michigan to be named one of the nation’s 15 Top Health Systems® by Truven Health Analytics for 2015. This is the fourth time the organization has received this recognition.
###
GPs and the Fit for Work scheme

|
An editorial by primary care researchers at Plymouth University Peninsula Schools of Medicine and Dentistry, and published today, Monday 29 June 2015 in the British Journal of General Practice, analyses the GP role in the sickness certification process and the new Fit for Work scheme and suggests that GPs are key to supporting individuals to maintain the hope and belief that they can work, “rather than adding to the numbers of individuals off work on long term sickness who may have been able to work.”
The Fit for Work Scheme will be introduced in most regions in England and Wales at the end of this month. Its aim is to provide additional support for those in employment at risk of long term incapacity by using an occupational health-based assessment and a plan for helping individuals return to work.
The GP’s role in the new voluntary scheme is advisory, supporting their patients to consider the benefits of extra support. This complements the recently introduced ‘fit note’ certificate that allows GPs to be clearer about their patients’ capacity to work and extra support that may help them return to work.
GPs have played a long-standing role in sickness certification which, since fit notes replaced sick notes in 2010, has focused of the cost of sickness leave and the health benefits of keeping people in work. Recent research has shown that this role is a challenging one with tension and anxiety for GP and patient alike. For example, put simply one study suggested that it was easier to get sickness certification if a patient presented with physical rather than psychological symptoms.
The authors of today’s editorial are hopeful that the Fit for Work scheme will help to address some of these tensions and anxieties, as well as provide valuable support to individuals to return to work who might otherwise have never been able to do so.
The editorial also identified potential benefits of certification for those who are not in employment. Fit notes allow GPs to provide helpful comments and a clear diagnosis as part of the certification process, which in turn validates an individual’s eligibility for the Employment and Support Allowance. This may also reduce the need for face-to-face assessments or work focused interviews.
Where an individual’s capacity for work is limited by illness, the authors suggest that the new scheme will provide appropriate support for returning to work. The use of the ‘may be fit for work’ tick box may well lead to useful conversations about an individual’s ability for work in the future, rather than defining someone as likely never to be able to work again. While this has huge potential for positive impact on an individual’s life, the editorial’s authors note caution and the need for sensitivity to avoid causing additional anxiety.
Lead author for the editorial, Professor Richard Byng from Plymouth University Peninsula Schools of Medicine and Dentistry, said: “Assessing and advising patients about the relationship between their health and their employment has always been a challenging one for GPs. Exclusion from work is not the most appropriate diagnosis for everyone, even if they do not agree with their doctor’s decision, and for some patients there are positive benefits to returning to work.”
He added: “If an individual is signed off for a period between four and 12 weeks, there is a greater chance they may never return to work. We would suggest that helping a patient to weigh up the pros and cons of returning to work is a vital role for the GP and would help to avoid the negative consequences of never returning to work, being signed off as medically unfit to work or simply being made redundant.
“Fit for Work and the 2010 fit notes put the GP in this central role. Our conclusion is that the GP can help patients to achieve the mind-set where they believe they can work. An outcome of this will be to reduce the number of people on long term sick leave who may have been able to work, with all the benefits that could bring to the individual, employers and the state.”
###
Andrew Gould
[email protected]
Experimental treatment sends deadly leukemia into remission
|
An experimental new treatment approach for a rare, deadly leukemia can send the disease into remission even in patients for whom the standard therapy has failed, buying them more time to have the stem cell transplant that could save their lives, a small pilot study has found.
“It was unbelievable, really, seeing a patient who had already failed Campath [the drug typically used to treat the disease] literally going back into remission,” said Thomas P. Loughran Jr., M.D., director of the University of Virginia Cancer Center and one of the leaders of the study. “We were able to get every single patient back into remission.”
The new approach to battling T-cell prolymphocytic leukemia combines immunotherapy - boosting the body’s immune system - with epigenetics, the manipulation of gene activity. It’s a cutting-edge combination that holds great promise not just for treating T-cell prolymphocytic leukemia but, possibly, many other cancers as well. “There’s been a revolution in the last few years seeing success with immunotherapy, and people speculated that perhaps if you combined epigenetic and immunotherapy, that might be even more spectacular,” Loughran said. “This is proof of principle that this might be true.”
The pilot study, led by Loughran at UVA and Elliot Epner, M.D., at Pennsylvania State University College of Medicine, looked at eight patients with T-cell prolymphocytic leukemia, an aggressive cancer that is extremely difficult to treat. It’s also extremely rare, appearing most commonly in older men.
The experimental approach did not cure the patients, but it did send them all into remission. And it worked repeatedly - patients could be re-treated and receive the same benefit, providing vital time as they looked for a suitable bone marrow/stem cell donor. (To receive a transplant for this disease, patients must first be in remission.)
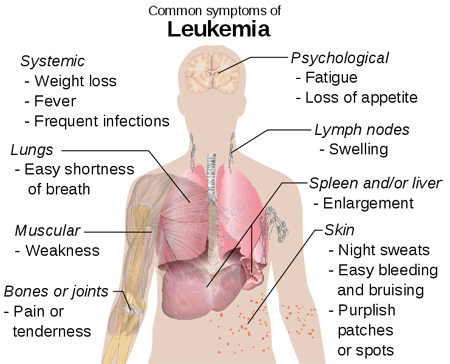 There are limitations to the experimental approach. Mounting toxicity limits how many times the treatment can be administered, and the suppression of the immune system can lead to infections and other complications. But the treatment made a significant difference for all the study participants. One patient was expected to live only four months but survived 34. Three others were still alive at the time the researchers were compiling the trial results.
There are limitations to the experimental approach. Mounting toxicity limits how many times the treatment can be administered, and the suppression of the immune system can lead to infections and other complications. But the treatment made a significant difference for all the study participants. One patient was expected to live only four months but survived 34. Three others were still alive at the time the researchers were compiling the trial results.
‘Unbelievable’ success for small pilot study
Treatment buys critical time for patients seeking potentially life-saving transplant
Cutting-edge combo pairs immune therapy, manipulation of gene activity
Drugs already approved by the Food and Drug Administration
Study ‘proof of principle’ for treating many other cancers as well
The drugs used in the treatment are already commercially available, meaning doctors could, in theory, administer the treatment without further testing. Loughran, however, believes there needs to be additional study, hopefully in a larger trial, but the rarity of the disease makes recruiting subjects difficult. As such, he encourages patients with the disease to consider seeking treatment at UVA. “We’d be very glad to see them here, if they want to come see us,” he said.
The study results have been published online by the journal Science Translational Medicine. The article was authored by Zainul S. Hasanali, Bikramajit Singh Saroya, August Stuart, Sara Shimko, Juanita Evans, Mithun Vinod Shah, Kamal Sharma, Violetta V. Leshchenko, Samir Parekh, Loughran and Epner.
###
Josh Barney
[email protected]
434-906-8864
Study could reduce unnecessary cancer screening

|
A large clinical trial led by researchers at The Ottawa Hospital and the University of Ottawa has found that contrary to expectations, a CT scan of the abdomen and pelvis does not improve cancer detection in people with unexplained blood clots in their legs and lungs. The results, published in the June 22 edition of the New England Journal of Medicine, are expected to improve patient care and reduce screening costs around the world.
More than 500,000 Canadians and Americans are diagnosed with blood clots in the lungs and legs each year (called venous thromboembolism). In some cases, the clots are caused by trauma, surgery prolonged immobility or a known cancer, but in about half of cases, the cause of the blood clots is unknown.
‘Unexplained blood clots have long been thought of as a possible early warning sign of cancer, with previous studies suggesting that up to 10 percent of patients with unexplained clots will be diagnosed with cancer within the year,’ explained Dr. Marc Carrier, lead author of the study and a hematologist and senior scientist at The Ottawa Hospital. ‘Some clinical guidelines recommend a CT scan of the abdomen and pelvis in these patients, in addition to other cancer screening, but there has been very little evidence to know if the added CT scan is helpful. We did this study to find out.’
The trial involved 854 patients in nine Canadian centres who had unexplained blood clots in the legs, lungs or both. Participants were randomized to receive basic cancer screening or basic cancer screening plus a CT scan of the abdomen and pelvis. Basic cancer screening included blood work and a chest X-ray, in addition to gender-specific screening (such as a breast exam, pap smear and prostate exam) if it had not been conducted in the last year.
The study showed that there was no difference in the number of new cancers detected in the two groups, with approximately four percent of patients from each group being diagnosed with cancer within the next year. There was also no difference in the number of cancer-associated deaths.
‘Although it is tempting to believe that more cancer screening is always better, our study shows that this is not necessarily the case, ’ said Carrier, who is also an associate professor at the University of Ottawa. ‘And in fact, unnecessary CT scanning has real risks. It can cause stress and anxiety in patients, as well as radiation exposure, and it can lead to over-investigation of false-positive findings. Our study means many patients will now be able to avoid this.’
The results could also lead to significant savings for the health-care system. Approximately 30,000 Canadians suffer an unexplained blood clot in the legs or lungs every year, and a CT scan costs approximately $300, resulting in a potential saving of $9M per year in Canada alone.
Jamie Dossett-Mercer participated in the clinical trial at the Ottawa Hospital after being diagnosed with an unexplained blood clot in the left leg in May 2013. Dossett-Mercer was in the group that received the CT scan. ‘I’m glad that I could contribute to research that will help patients and save the health-care system money,’ he said. ‘I’m also glad to know that these tests are not required. When you are diagnosed with a serious illness you are already going through so many tests and worrying so much, so you really don’t want to be doing extra tests if they aren’t helpful.’
The study’s senior author, Dr. Marc Rodger, noted that the four percent incidence of cancer observed in this study was lower than the 10 percent found in previous studies, possibly because of improvements in other kinds of cancer screening in the general population. ‘It is very reassuring to know that the risk of cancer is less than we thought in these patients,’ said Rodger, also a hematologist and senior scientist at The Ottawa Hospital and professor at the University of Ottawa. ‘It means I can have a very different kind of conversation with my newly-diagnosed patients.’
The paper, titled ‘Screening for occult cancer in unprovoked venous thromboembolism’ was published in the New England Journal of Medicine on June 22, 2015 and is authored by Carrier M, Lazo-Langner A, Shivakumar S, Tagalakis V, Zarychanski R, Solymoss S, Routhier N, Douketis J, Danovitch K, Lee AY, Le Gal G, Wells PS, Corsi DJ, Ramsay T, Coyle D, Chagnon I, Kassam Z, Tao H, and Rodger MA. The results were also presented on June 22 at the International Society of Thrombosis and Hemostasis meeting in Toronto, Canada.
This research was supported by the Heart and Stroke Foundation of Canada and The Ottawa Hospital Foundation.
‘The Heart and Stroke Foundation is committed to funding research excellence with the power to create more survivors,’ says Mary Lewis, VP Research and Knowledge Exchange for the Heart and Stroke Foundation. ‘Thanks to the generosity of our donors, we can continue to fund leading research like this which will improve the health of Canadians, while saving our system valuable health dollars.’
###
For more information, please contact:
Lois Ross
[email protected]
Office: 613-737-8899 x73687 or Cell: 613-297-8315
Ottawa Hospital Research Institute
About Ottawa Hospital Research Institute
The Ottawa Hospital Research Institute is the research arm of The Ottawa Hospital and is an affiliated institute of the University of Ottawa, closely associated with its faculties of Medicine and Health Sciences. The Ottawa Hospital Research Institute includes more than 1,700 scientists, clinical investigators, graduate students, postdoctoral fellows and staff conducting research to improve the understanding, prevention, diagnosis and treatment of human disease. Support our research. Give to the Tender Loving Research campaign.
The University of Ottawa - A crossroads of cultures and ideas The University of Ottawa is home to over 50,000 students, faculty and staff, who live, work and study in both French and English. Our campus is a crossroads of cultures and ideas, where bold minds come together to inspire game-changing ideas. We are one of Canada’s top 10 research universities - our professors and researchers explore new approaches to today’s challenges. One of a handful of Canadian universities ranked among the top 200 in the world, we attract exceptional thinkers and welcome diverse perspectives from across the globe.
###
Lois Ross
[email protected]
613-737-8899 x73687
Study shows global warming is unlikely to reduce winter deaths

|
A study by researchers at Columbia University’s Mailman School of Public Health debunks the assumption that global warming will lead to a decline in the number of deaths in winter. Findings by Professor Patrick Kinney, ScD, professor of Environmental Health Sciences and director of the School’s Climate and Health Program, showed that a warming climate trend led to much smaller reductions in cold-related mortality than some experts have anticipated. Among 39 cities in the U.S. and France, there was no evidence that cities having warming temperatures experienced any less winter mortality than did cooler cities.
“Some have claimed that warmer winters due to climate change will lead to big reductions in winter deaths. Our work suggests that this is unlikely to be the case,” said Dr. Kinney, who was a lead author on the recent report from the Intergovernmental Panel on Climate Change and also serves on the New York City Panel on Climate Change.
If cold temperatures were directly responsible for winter mortality rates, then we would expect future warming to lead to substantial reductions in winter mortality, according to Dr. Kinney. On the other hand, “climate warming would have little benefit if seasonal factors other than temperature are mainly responsible for winter excess mortality,” he noted.
To determine whether and to what extent cold temperatures affect excess winter mortality, Dr. Kinney and colleagues analyzed temperature and mortality data from 36 U.S. cities and Paris, Lyon, and Marseille in France. Mortality rates were obtained from the U.S. National Center for Health Statistics and the French National Institute for Statistics and Economics Studies for the period 1971-2007. Findings showed that cities with warmer winters have similar rates of winter deaths compared to their colder winter-counterparts and that there was little relationship evident between mortality and cold temperatures.
“These cities vary widely in demography, urban design, and socio-cultural background, all of which might influence exposure to outdoor temperature and related mortality risks,” said Dr. Kinney.
The lack of correlation between seasonal temperature differences and winter season excess mortality suggests that other seasonal factors are driving winter excess mortality including lack of exercise, low humidity and time spent indoors which may lead to increased risk of flu and other respiratory infections and its complications.
###
Co-authors are Elisaveta Petkova of the Mailman School of Public Health; Joel Schwartz of the Harvard School of Public Health; Mathilde Pascal, Alain Le Tertre, and Sylvia Medina at the Institut de Veille Sanitaire; and Robert Vautard at the Laboratoire des Sciences du Climat et de l’Environment.
The study was supported by the U.S. National Oceanic and Atmospheric Administration (grant NA100AR4310212) and the U.S. National Institute of Environmental Health Sciences (grant P30 ES09089). Additional support was provided by the Earth Institute at Columbia University. The authors reported no conflicts of interest.
About Columbia University’s Mailman School of Public Health
Founded in 1922, Columbia University’s Mailman School of Public Health pursues an agenda of research, education, and service to address the critical and complex public health issues affecting New Yorkers, the nation and the world. The Mailman School is the third largest recipient of NIH grants among schools of public health. Its over 450 multi-disciplinary faculty members work in more than 100 countries around the world, addressing such issues as preventing infectious and chronic diseases, environmental health, maternal and child health, health policy, climate change & health, and public health preparedness. It is a leader in public health education with over 1,300 graduate students from more than 40 nations pursuing a variety of master’s and doctoral degree programs. The Mailman School is also home to numerous world-renowned research centers including ICAP (formerly the International Center for AIDS Care and Treatment Programs) and the Center for Infection and Immunity.
Massively parallel gene function assays aim to reduce uncertainty of genetic diagnoses

|
Patients seeking certainty in genetic tests often receive a perplexing result. Many learn they carry a ‘variant of unknown significance’ of a disease-linked gene. Such variants might—or equally might not—increase disease risk.
A study published in the June issue of the journal Genetics characterized nearly 2000 variants of the breast cancer-associated gene BRCA1, demonstrating the potential of a new approach for sorting out which variants are harmful and which are harmless.
Because genetic tests increasingly use more comprehensive multi-gene and whole-genome sequencing methods, it’s becoming more common for patients to learn they carry a variant of unknown significance. For example, a 2014 study showed 42 percent of breast cancer patients who received results from a 25-gene hereditary cancer genetic test carried a variant of unknown significance in one of the scanned genes.
‘There’s not much you can do with this information, except worry,’ says lead author Lea Starita of the University of Washington. ‘We hope to reduce some of the uncertainty by driving forward technologies for efficient functional testing of gene variants.’
The team used the BRCA1 gene as a test case for their approach because more is known about the functions and sequence variants of BRCA1 than many other genes associated with disease.
Normally, BRCA1 codes for a protein that regulates how the body repairs DNA mutations. People who carry a known pathogenic (disease-linked) BRCA1 variant have a higher risk of breast and ovarian cancers because the encoded protein is faulty; it fails to properly regulate DNA repair and allows cancer-causing mutations to accumulate.
But not all BRCA1 variants are pathogenic. Scientists can’t usually tell whether a gene variant confers a higher disease risk until enough people with the variant have been identified to allow statistical analysis of their disease rates. For extremely rare or unique variants, such studies might never be possible.
To understand more about new or rare variants, the authors proposed an approach that doesn’t directly examine disease risks, but instead measures the function of the gene’s protein product. The encoded protein is tested with relatively simple laboratory assays that gauge whether the protein retains its normal biochemical functions. By performing many thousands of these tests at once, biologists can assess all possible variants of a gene quickly and efficiently. This method of performing protein function assays in a massively parallel format is called ‘deep mutational scanning.’
Such laboratory tests are not perfect measures of whether or not a particular variant is functional. For example, proteins sometimes behave differently inside the human body than they do in a test tube, a laboratory organism, or a cell growing in a dish. But the large amounts of data generated by such experiments are still useful to researchers. For example, a database of functional information could help them to prioritize variants for more detailed studies, or to provide preliminary classifications of newly discovered variants.
In this study, the team combined data from two different tests of a key part of the BRCA1 protein called the RING domain. Around 58 percent of known pathogenic BRCA1variants affect this part of the protein. One of the tests measured the ability of the RING domain to attach small proteins called ubiquitin tags to other proteins. The second test measured whether the RING domain could bind to part of another protein called BARD1 when both proteins were produced in a yeast cell. If BRCA1 cannot bind to BARD1, it no longer prevents tumor formation. The data from both massively parallel assays were largely consistent with previous studies.
Combined scores from the massively parallel tests were also used to predict results from the so-called ‘gold standard’ of BRCA1 functional assays. This more comprehensive test assesses the full-length BRCA1 protein’s ability to regulate DNA repair in cells, and is the measure that best correlates with disease risk in patients. The researchers found they could use data from the deep mutational scan to predict how a variant would perform in the gold standard test. The predictions made in this way were substantially more reliable than those made by widely-used computational methods that are currently used in genomic studies to predict the severity of mutations.
Starita cautions that although the results show remarkable promise, the data are not yet ready for use in the clinic. ‘Clinicians can’t use the data in isolation to make conclusions about a variant,’ says Starita. ‘Our model, based on experimental data, is a better predictor of the effects of mutations than those based on purely computational methods, but it is still not perfect.’
The team is working on related large-scale approaches for other genes. For example, many genetic variants linked to autism are located in genes that alter the packaging of DNA into a compact form called chromatin. The researchers are developing massively-parallel assays for chromatin remodeling that could be used to assess the function of many autism-associated variants.
The researchers are also using new genome editing technologies to create thousands of genetic variants directly in the genomes of cells growing in culture. These technologies would allow many other biochemical tests of protein function - such as protein-protein interaction, enzyme catalysis, and protein stability - to be performed at enormous scales, even for relatively poorly characterized genes.
‘As genetic testing becomes both cheaper and more comprehensive, we will need a variety of approaches to translate the deluge of genetic data into practical information on individual health risks,’ says Starita. ‘Deep mutational scans are one tool to help meet this urgent need.’
###
Citation: Lea M. Starita, David L. Young, Muhtadi Islam, Jacob O. Kitzman, Justin Gullingsrud, Ronald J. Hause, Douglas M. Fowler, Jeffrey D. Parvin, Jay Shendure, and Stanley Fields (2015). Massively parallel functional analysis of BRCA1 RING domain variants. Genetics 200(2):413-422 doi: 10.1534/genetics.115.175802
About the Genetics Society of America (GSA)
Founded in 1931, the Genetics Society of America (GSA) is the professional scientific society for genetics researchers and educators. The Society’s more than 5,000 members worldwide work to deepen our understanding of the living world by advancing the field of genetics, from the molecular to the population level. GSA promotes research and fosters communication through a number of GSA-sponsored conferences including regular meetings that focus on particular model organisms. GSA publishes two peer-reviewed, peer-edited scholarly journals: Genetics, which has published high quality original research across the breadth of the field since 1916, and G3:Genes|Genomes|Genetics, an open access journal launched in 2011 to disseminate high quality foundational research in genetics and genomics. The Society also has a deep commitment to education and fostering the next generation of scholars in the field.
###
Tracey DePellegrin
[email protected]
412-760-5391
Academies make recommendations for improving public health

|
In recent decades, enormous successes have been achieved in the field of public health. Three examples of these are the fight against HIV, the reduction in cardiovascular disease, and protection for non-smokers. For Germany to make even better use of the potential of public health, it needs more political support, improved research structures, and stronger international involvement. The German National Academy of Sciences Leopoldina, acatech - the National Academy of Science and Engineering, and the Union of the German Academies of Sciences and Humanities point this out in a joint statement entitled “Public Health in Germany - Structures, Developments and Global Challenges”, published today.
Public health is the science and practice of preventing disease, prolonging life, and improving quality of life across an entire population. The concept covers the general promotion of health via comprehensive, organised measures at all levels of society. Research questions and measures related to public health affect all sectors of the healthcare system, the education and social systems, and parts of the economy. Germany is doing outstanding research on various aspects of public health. However, the structures in research, teaching and practice are not yet optimally developed - especially considering the major international challenges that exist. In their “Public Health in Germany” statement, the academies make recommendations on how the field can be improved in Germany.
(1) The academies’ recommendations for education and further training include: improving collaboration between public health researchers, the public healthcare service, public health practitioners, and the public; coordinating professional education goals at national level; establishing interdisciplinary training schemes; opening up new career paths in public health; and incorporating elements of public health into the curricula of all medical professions. Public health professions should be made more attractive and more respected career options.
(2) The quality and interdisciplinarity of research must improve. The academies also recommend a research agenda to develop political measures and programmes for improving health, and to strengthen the healthcare system. The currently underused potential of cohort and randomised studies should be exploited, in particular to investigate the impact of public health measures. The academies recommend examining legislative proposals on data protection in Germany and the EU to establish whether they might place new and avoidable hurdles in the way of health research.
(3) With regard to implementing research findings in practice, the academies recommend public dialogue and, in particular, building strategic links between science, the public healthcare service, policymakers, the healthcare sector and civil society. These activities should also extend to EU level and to global cooperation in the field of global health.
(4) The academies list four options for structural reforms that will strengthen public health in Germany: a network with competitive financing; a virtual coordinating body; a public health institute; and a centre for public and global health that would steer all activities in this field.
The “Public Health in Germany” statement was produced by an interdisciplinary working group made up of scientists from Germany, Switzerland, France, the Netherlands and the UK. The experts come from all fields of public health, including economics, the social sciences, medical fields such as infection research and genetics, health services research, and research into global health issues.
###
“Public Health in Germany - Structures, Developments and Global Challenges” - A statement by the German National Academy of Sciences Leopoldina, acatech - the National Academy of Science and Engineering, and the Union of the German Academies of Sciences and Humanities, 82 pages, ISBN: 978-3-8047-3345-9
The German National Academy of Sciences Leopoldina, acatech - National Academy of Science and Engineering, and the Union of the German Academies of Sciences and Humanities provide policymakers and society with independent, science-based advice on issues of crucial importance for our future. The Academies’ members are outstanding researchers from Germany and abroad. Working in interdisciplinary working groups, they draft statements that are published in the series of papers Schriftenreihe zur Wissenschaftsbasierten Politikberatung (Monograph Series on Science-based Policy Advice) after being externally reviewed and subsequently approved by the Standing Committee of the German National Academy of Sciences Leopoldina.
###
Caroline Wichmann
[email protected]
49-345-472-39800
UA researchers discover component of cinnamon prevents colorectal cancer in mice

|
Research conducted at the University of Arizona College of Pharmacy and the UA Cancer Center indicates that a compound derived from cinnamon is a potent inhibitor of colorectal cancer.
Georg Wondrak, Ph.D., associate professor, and Donna Zhang, Ph.D., professor, both of the UA College of Pharmacy Department of Pharmacology and Toxicology, recently completed a study in which they proved that adding cinnamaldehyde, the compound that gives cinnamon its distinctive flavor and smell, to the diet of mice protected the mice against colorectal cancer. In response to cinnamaldehyde, the animals’ cells had acquired the ability to protect themselves against exposure to a carcinogen through detoxification and repair.
‘This is a significant finding,’ says Zhang, who, along with Wondrak, is a member of the UA Cancer Center. ‘Because colorectal cancer is aggressive and associated with poor prognoses, there is an urgent need to develop more effective strategies against this disease.’
‘Given cinnamon’s important status as the third-most-consumed spice in the world,’ Wondrak adds, ‘there’s relatively little research on its potential health benefits. If we can ascertain the positive effects of cinnamon, we would like to leverage this opportunity to potentially improve the health of people around the globe.’
Drs. Wondrak and Zhang’s study, ‘Nrf2-dependent suppression of azoxymethane/dextrane sulfate sodium-induced colon carcinogenesis by the cinnamon-derived dietary factor cinnamaldehyde,’ has been published online and will appear in a print issue of Cancer Prevention Research later this spring.
A story about the cinnamaldehyde study appears on the UA College of Pharmacy’s website.
The next step in the research is to test whether cinnamon, as opposed to cinnamaldehyde, prevents cancer using this same cancer model. Because cinnamon is a common food additive already considered safe - it’s not a synthetic, novel drug - a study in humans may not be too far off.
Wondrak outlines questions to investigate going forward: ‘Can cinnamon do it, now that we know pure cinnamaldehyde can? And can we use cinnamaldehyde or cinnamon as a weapon to go after other major diseases, such as inflammatory dysregulation and diabetes? These are big questions to which we might be able to provide encouraging answers using a very common spice.’
###
About the UA College of Pharmacy
Established in 1947, the University of Arizona College of Pharmacy was the first health sciences college at the Tucson campus of the University of Arizona. Educating pharmacists and pharmaceutical scientists, the college participates in many interdisciplinary and multi-institutional educational and research collaborations throughout Arizona and globally. It is ranked among the premier colleges of pharmacy in the United States and is routinely among the top 20 colleges of pharmacy in terms of external funding for research, including funding from the National Institutes of Health.
Research reported in this release was supported by the National Cancer Institute of the National Institutes of Health under grant number 5R21CA166926-02.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
###
Large doses of antioxidants may be harmful to neuronal stem cells

|
Stem cells are especially sensitive to oxygen radicals and antioxidants shows new research from the group of Anu Wartiovaara in the Molecular Neurology Research Program of University of Helsinki. The research led by researcher Riikka Martikainen was published in Cell Reports -journal May 28th 2015.
Mitochondria are cellular power plants that use oxygen to produce energy. As a by-product they produce reactive oxygen. Excessive oxygen radicals may cause damage to cells but they are needed in small quantities as important cellular signaling molecules. One of their main functions is to control function of stem cells. Antioxidants are widely used to block the damage caused by reactive oxygen. To enhance their effect some new antioxidants are targeted to accumulate into mitochondria.
The current research showed that a small increase in oxygen radicals did not directly lead to cellular damage but disrupted intracellular signaling in stem cells and lead to decrease in their stemness properties. Treatment with antioxidants was able to improve the stemness properties in these cells. However, surprisingly, the researchers found that an antioxidant targeted to mitochondria showed dose-dependent toxic effects especially on neural stem cells.
The use of antioxidants as dietary supplements is common, but little is known of their effects on stem cells. This new research shows that large doses of antioxidants may be harmful to neural stem cells. Additional research on stem cells should be done to assess safety of mitochondria targeted antioxidants.
###
Article: Hämäläinen RH, Ahlqvist KJ, Ellonen P, Lepistö M, Logan A, Otonkoski T, Murphy MP, Suomalainen A. MtDNA Mutagenesis Disrupts Pluripotent Stem Cell Function by Altering Redox Signaling. Cell Reports 2015
###
Riikka Martikainen
[email protected]
358-947-171-965
Journal
Cell Reports
As death rates drop, nonfatal diseases and injuries take a bigger toll on health globally

|
People across the world are living longer but spending more time in ill health as rates of nonfatal diseases and injuries - including diabetes and hearing loss - decline more slowly than death rates, according to a new analysis of 301 diseases and injuries in 188 countries.
Using a measurement known as years lived with disability, or YLDs, researchers from around the world quantified the impact of health problems that impair mobility, hearing, or vision, or cause pain in some way but aren’t fatal. In 2013, low back pain and major depressive disorder were among the 10 leading causes of YLDs in every country. Other leading causes globally included neck pain, anxiety disorders, migraine headaches, and diabetes. The leading causes of years lived with disability have remained largely the same during this period, but they are taking an increased toll on health due to population growth and aging.
YLDs per person increased in 139 of 188 countries between 1990 and 2013, meaning that more people are spending more time in poor health. Musculoskeletal disorders, combined with fractures and soft tissue injuries, accounted for one-fifth of YLDs globally in 2013, ranging from 11% in Mali to 30% in South Korea. Mental and substance abuse disorders also caused 20% of YLDs globally, ranging from 15% in Germany to 37% in Qatar.
“Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013” is the first study to examine the extent, pattern, and trends of nonfatal health loss across countries. Published in The Lancet on June 8, the study was conducted by an international consortium of researchers working on the Global Burden of Disease project and led by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington.
“Many countries around the world have made great progress in addressing fatal diseases, but nonfatal illnesses pose the next major threat in terms of disease burden,” said Professor Theo Vos of IHME, the study’s lead author. “This need to meet the challenge of nonfatal diseases and injuries only becomes more urgent as the population increases and people live longer.”
Between 1990 and 2013, YLDs increased globally from 537.6 million in 1990 to 764.8 million in 2013 for both sexes. Men and women around the world share the same leading causes of YLDs, with the exception of schizophrenia as a leading cause for men and other musculoskeletal disorders for women. Musculoskeletal disorders, mental and substance use disorders, neurological disorders, and chronic respiratory conditions were the main drivers of YLDs in 2013. The disease burdens of both low back pain and depression have increased more than 50% since 1990.
 Researchers found that as people aged they experienced a greater number of ailments resulting from nonfatal diseases and injuries. Many people also suffered from multiple conditions at the same time. The number of people who suffered from 10 or more ailments increased by 52%. And it’s not just the elderly who are affected. Although the impact of YLDs increases with age, of the 2.3 billion people who suffered from more than five ailments, 81% of them were younger than 65 years old.
Researchers found that as people aged they experienced a greater number of ailments resulting from nonfatal diseases and injuries. Many people also suffered from multiple conditions at the same time. The number of people who suffered from 10 or more ailments increased by 52%. And it’s not just the elderly who are affected. Although the impact of YLDs increases with age, of the 2.3 billion people who suffered from more than five ailments, 81% of them were younger than 65 years old.
A relatively small number of diseases have a massive impact, researchers found. Just two acute diseases - affecting people for less than three months - caused more than 20 billion new cases of disease globally in 2013: upper respiratory infections (18.8 billion) and diarrheal diseases (2.7 billion). And just eight causes of chronic diseases - affecting people for three months or longer - impacted more than 10% of the world’s population. These included tension-type headaches and iron-deficiency anemia.
In 2013, war and conflict was a leading cause of YLDs in several countries as well, including El Salvador, Lebanon, Guatemala, Peru, and Syria. In three countries - Cambodia, Nicaragua, and Rwanda - war was the top cause of years lived with disability. Other notable causes of YLDs in different regions included falls (Central Europe), asthma (a top-10 cause in many Latin American countries), and opioid dependence (a top-five cause in several Middle Eastern countries). Nonfatal conditions are not yet becoming the dominant source of disease burden in sub-Saharan Africa as they are in other parts of the world, but their impact has grown since 1990.
“What ails you isn’t necessarily what kills you,” said IHME Director Dr. Christopher Murray. “As nonfatal illnesses and related ailments affect more people of all ages, countries must look closely at health policies and spending to target these conditions.”
Leading causes of YLDs globally for both sexes in 2013
Low back pain
Major depressive disorder
Iron-deficiency anemia
Neck pain
Age-related and other hearing loss
Diabetes mellitus
Migraine
Chronic obstructive pulmonary disease
Anxiety disorders
Other musculoskeletal disorders
Leading causes of YLDs globally for men in 2013
Low back pain
Major depressive disorder
Age-related and other hearing loss
Iron-deficiency anemia
Diabetes mellitus
Neck pain
Chronic obstructive pulmonary disease
Migraine
Anxiety disorders
Schizophrenia
Leading causes of YLDs globally for women in 2013
Low back pain
Major depressive disorder
Iron-deficiency anemia
Neck pain
Migraine
Other musculoskeletal disorders
Anxiety disorders
Age-related and other hearing loss 9 Diabetes mellitus 10 Chronic obstructive pulmonary disease
###
Download the study at http://www.healthdata.org/research-article/global-regional-and-national-incidence-prevalence-and-years-lived-disability-2013.
The Institute for Health Metrics and Evaluation (IHME) is an independent global health research organization at the University of Washington that provides rigorous and comparable measurement of the world’s most important health problems and evaluates the strategies used to address them. IHME makes this information widely available so that policymakers have the evidence they need to make informed decisions about how to allocate resources to best improve population health.
Media contact:
Rhonda Stewart, IHME
[email protected]
+1-206-897-2863
###
Drug prevents passage of HBV during pregnancy
|
|
The antiviral drug telbivudine prevents perinatal transmission of hepatitis B virus (HBV), according to a study1 in the June issue of Clinical Gastroenterology and Hepatology, the official clinical practice journal of the American Gastroenterological Association.
“If we are to decrease the global burden of hepatitis B, we need to start by addressing mother-to-infant transmission, which is the primary pathway of HBV infection,” said study author Yuming Wang from Institute for Infectious Diseases, Southwest Hospital, Chongqing, China. “We found that telbivudine not only eliminated vertical transmission of HBV from pregnant women to theirs infants, but that it is also safe and well tolerated by women and infants.”
Researchers performed a prospective study of 450 HBV-positive pregnant women with high viral load, or significant HBV in the blood, during the second or third trimester of pregnancy. Two hundred and seventy nine women received telbivudine (600 mg daily) during weeks 24 through 32 of gestation, and 171 women who were unwilling to take antiviral drugs participated as controls. At six months after birth, none of the infants whose mothers were given telbivudine tested positive for HBV, compared to 14.7 percent of infants in the control group.
Levels of HBV also decreased for the moms: almost a quarter who received telbivudine had no HBV detectable in their system. Those not on the antiviral medication all tested positive for HBV. A significantly higher proportion of women given telbivudine had undetectable levels of HBV DNA in cord blood (99.1 percent) than controls (61.5 percent). No severe adverse events or complications were observed in women or infants.
The long-term influence of using telbivudine, especially when compared to the other recommended oral antiviral drug, tenofovir, remains to be explored.
Hepatitis B virus, which has infected nearly two billion people worldwide, is a leading cause of liver disease. Learn more about hepatitis in the AGA patient brochure.
###
The authors have no commercial associations or conflicts to disclose.
1 Wu, Quanxin, et al. Telbivudine Prevents Vertical Transmission of Hepatitis B Virus From Women With High Viral Loads: A Prospective Long-Term Study, Clinical Gastroenterology and Hepatology, Volume 13(6): 1170-1176. http://www.cghjournal.org/article/S1542-3565(14)01356-1/abstract
About the AGA Institute
The American Gastroenterological Association is the trusted voice of the GI community. Founded in 1897, the AGA has grown to include more than 16,000 members from around the globe who are involved in all aspects of the science, practice and advancement of gastroenterology. The AGA Institute administers the practice, research and educational programs of the organization..
About Clinical Gastroenterology and Hepatology
The mission of Clinical Gastroenterology and Hepatology is to provide readers with a broad spectrum of themes in clinical gastroenterology and hepatology. This monthly peer-reviewed journal includes original articles as well as scholarly reviews, with the goal that all articles published will be immediately relevant to the practice of gastroenterology and hepatology. For more information, visit http://www.cghjournal.org.
###
Rachel Steigerwald
[email protected]
301-272-1603
Study shows treatment for genetically caused emphysema is effective
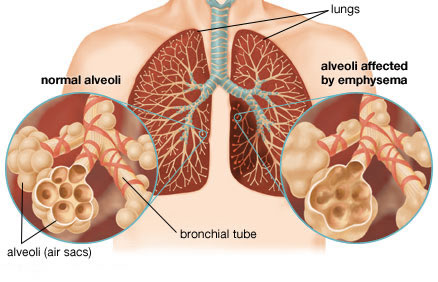
|
A landmark clinical study in the Lancet provides convincing evidence that a frequently overlooked therapy for genetically-caused emphysema is effective and slows the progression of lung disease.
Alpha-1 antitrypsin deficiency is an inherited disorder that can cause emphysema even without exposure to tobacco smoke. Alpha-1 antitrypsin (AAT) is a protein made in the liver that protects the lungs. With this disorder, the AAT protein builds up in liver cells and doesn’t reach the lungs to protect them. Augmentation therapy involves regular infusions of purified AAT protein to raise the level of the protein in the blood and lungs. Although the therapy has been available for more than 25 years, it has seen limited use because doctors have been unsure that it works.
The study, “Intravenous augmentation treatment and lung density in severe α1 antitrypsin deficiency (RAPID): a randomised, double-blind, placebo-controlled trail,” published online today will change how clinicians understand this treatment and encourage them to consider its early use before the condition causes severe emphysema.
By using CT scans to measure the lung density of patients in the trial, the researchers were able to overcome some of the challenges that have been associated with studying the effectiveness of the treatment. “This treatment has now been studied in our centre using the most sensitive measure of lung structure - a radiologic measurement of lung density - allowing us to detect changes far earlier than can be seen with standard breathing tests,” said Dr. Kenneth Chapman, Director of the Asthma and Airways Centre at Toronto Western Hospital and the Canadian research lead for the multicentre trial. “We can now say with certainty that augmentation therapy is effective and should be given to patients with emphysema caused by this deficiency.”
According to the Canadian Medical Association Journal, up to five per cent of people with chronic obstructive pulmonary disease (COPD) are thought to have alpha-1 antitrypsin deficiency, yet only four to five per cent of those with a deficiency have been identified. Even when the deficiency is diagnosed, there has typically been a delay of five to 10 years before this specific genetic problem has been identified as the cause of respiratory problems.
“Augmentation therapy not only preserves lung structure, but likely adds years of life,” said Dr. Chapman. “Patients with this condition need access to timely diagnosis and treatments to ensure they receive the best possible care”. Dr. Chapman added that this treatment is used only for this specific type of emphysema and is not of benefit to those with more common types of emphysema, chronic bronchitis or COPD.
Patients, like Ken Bee, who have been diagnosed with α1 antitrypsin deficiency, welcome the news that augmentation therapy is an effective treatment. Ken was diagnosed seven years ago and since receiving augmentation therapy his lung function has not decreased. “Without this treatment my symptoms would have progressed,” says Bee. “My hope is that more people will recognize the benefit it has to patients.”
###
About Toronto Western Hospital
Toronto Western Hospital has been serving the health care needs of its culturally diverse local community for more than 100 years. Home to the Krembil Neuroscience Centre, one of the largest combined clinical and research neurological facilities in North America, the Toronto Western Hospital is a leader in medical research and also offers expertise in community and population health and musculoskeletal health and arthritis. The Toronto Western Hospital, along with the Princess Margaret Cancer Centre, Toronto General Hospital and Toronto Rehabilitation Institute, is a member of the University Health Network and is affiliated with the University of Toronto.
###
Hearing impairment higher among Hispanic/Latino men, older individuals
|
Hearing impairment was more prevalent among men and older individuals in a study of U.S. Hispanic/Latino adults, according to a report published online by JAMA Otolaryngology-Head and Neck Surgery.
Hearing impairment is a common chronic condition that affects adults. Hearing impairment may lead to lower quality of life and is associated with an increased risk for dementia. Most hearing impairment is undiagnosed and untreated.
Karen J. Cruickshanks, Ph.D., of the University of Wisconsin, Madison, and co-authors determined the prevalence of hearing impairment among Hispanic/Latino adults from diverse backgrounds and identified the factors associated with hearing impairment.
The authors used data from the Hispanic Community Health Study/Study of Latinos, a population-based sample of Hispanic/Latinos from New York, Chicago, Miami, and San Diego, Calif. The study examined 16,415 self-identified Hispanic/Latino individuals who were between the ages of 18 and 74.
Overall, the study found 15 percent of participants had hearing impairment and about half of them (8.24 percent) had hearing loss in both ears (bilateral hearing impairment). In general, the prevalence of hearing impairment was higher among men and adults 45 and older. Among people 45 and older, hearing impairment was higher ranging by Hispanic/Latino background from 29.35 percent for men with Dominican background to 41.20 percent for Puerto Rican men, and from 17.89 percent for women of Mexican background to 32.11 percent for women reporting a mixed Hispanic/Latino background. The odds of hearing impairment were lower if individuals were more educated and had higher incomes. Also, noise exposure, diabetes and prediabetes were associated with hearing impairment, according to the results.
‘Future longitudinal studies of Hispanics/Latinos from diverse backgrounds could strengthen the determination of the risks associated with hearing loss. This longitudinal information is needed to identify modifiable risk factors to slow the progression of hearing loss with aging and to develop culturally appropriate effective intervention strategies to meet the communication needs of the Hispanic/Latino community,’ the study concludes.
###
(JAMA Otolaryngol Head Neck Surg. Published online May 28, 2015. doi:10.1001/.jamaoto.2015.0889. Available pre-embargo to the media at http://media.jamanetwork.com.)
Editor’s Note: this study includes funding/support disclosures. Please see article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
To contact corresponding author Karen J. Cruickshanks, Ph.D., call:
Emily Kumlien
[email protected]
608-265-8199
To place an electronic embedded link to this study in your story (links will be live at the embargo time): http://archotol.jamanetwork.com/article.aspx?doi=10.1001/jamaoto.2015.0889
###
Emily Kumlien
[email protected]
608-265-8199
The JAMA Network Journals
Designing better medical implants
|
Biomedical devices that can be implanted in the body for drug delivery, tissue engineering, or sensing can help improve treatment for many diseases. However, such devices are often susceptible to attack by the immune system, which can render them useless.
A team of MIT researchers has come up with a way to reduce that immune-system rejection. In a study appearing in the May 18 issue of Nature Materials, they found that the geometry of implantable devices has a significant impact on how well the body will tolerate them.
Although the researchers expected that smaller devices might be better able to evade the immune system, they discovered that larger spherical devices are actually better able to maintain their function and avoid scar-tissue buildup.
“We were surprised by how much the size and shape of an implant can affect its triggering of an immune response. What it’s made of is still an important piece of the puzzle, but it turns out if you really want to have the least amount of scar tissue you need to pick the right size and shape,” says Daniel Anderson, the Samuel A. Goldblith Associate Professor in MIT’s Department of Chemical Engineering, a member of MIT’s Koch Institute for Integrative Cancer Research and Institute for Medical Engineering and Science (IMES), and the paper’s senior author.
The researchers hope to use this insight to further develop an implantable device that could mimic the function of the pancreas, potentially offering a long-term treatment for diabetes patients. It could also be applicable to devices used to treat many other diseases.
“I believe the understanding achieved here will help scientists not only move forward on creating better implants to someday treat diabetes, but will also aid in the design of any type of human or animal implant to treat or diagnose disease,” says study author Robert Langer, the David H. Koch Institute Professor at MIT and a member of the Koch Institute, IMES, and the Department of Chemical Engineering.
Lead authors of the paper are Koch Institute postdocs Omid Veiseh and Joshua Doloff, and Minglin Ma, a former Koch Institute postdoc who is now an assistant professor at Cornell University.
Implanting cells
This study grew out of the researchers’ efforts to build an artificial pancreas, which began several years ago. The goal is to deliver pancreatic islet cells encapsulated within a particle made of alginate—a polysaccharide naturally found in algae—or another material. These implanted cells could replace patients’ pancreatic islet cells, which are nonfunctional in Type I diabetes.
Just like normal islet cells, these cells would sense sugar levels in the blood and secrete the appropriate amount of insulin to absorb the sugar, eliminating the need for insulin injections. However, if scar tissue surrounds the implanted cells, they can’t do their job.
“The purpose of these implantable devices is to protect the cells from the immune system, but allow them to stay alive and continue to function,” Anderson says.
The researchers tested spheres in two sizes—0.5 and 1.5 millimeters in diameter. In tests of diabetic mice, the spheres were implanted within the abdominal cavity and the researchers tracked their ability to accurately respond to changes in glucose levels. The devices prepared with the smaller spheres were completely surrounded by scar tissue and failed after about a month, while the larger ones were not rejected and continued to function for more than six months.
The larger spheres also evaded the immune response in tests in nonhuman primates. Smaller spheres implanted under the skin were engulfed by scar tissue after only two weeks, while the larger ones remained clear for up to four weeks. “We observed over an order of magnitude fewer immune cells on all surfaces of larger diameter spheres,” Doloff says.
“When we first got this data it was counterintuitive,” Anderson says. “There was reason to think when you have these little small beads they would elicit less of a response, but it just wasn’t the case.”
This effect was seen not only with alginate, but also with spheres made of stainless steel, glass, polystyrene, and polycaprolactone, a type of polyester.
“We realized that regardless of what the composition of the material is, this effect still persists, and that made it a lot more exciting because it’s a lot more generalizable,” Veiseh says.
Size and shape
The researchers believe this finding could be applicable to any other type of implantable device, including drug-delivery vehicles and sensors for glucose and insulin, which could also help improve diabetes treatment. Optimizing particle size and shape could also help guide scientists in developing other types of implantable cells for treating diseases other than diabetes.
“For any of these devices that people want to make, it may be important to think carefully about the size and shape of them,” Anderson says.
###
The research was funded by the Juvenile Diabetes Research Foundation, the Leona M. and Harry B. Helmsley Charitable Trust Foundation, the National Institutes of Health, the Koch Institute Support Grant from the National Cancer Institute, and the Tayebati Family Foundation. Veiseh was also supported by the Department of Defense.
###
Sarah McDonnell
[email protected]
617-253-8923
Single low-magnitude electric pulse successfully fights inflammation

|
The Feinstein Institute for Medical Research, the research arm of the North Shore-LIJ Health System, and SetPoint Medical Inc., a biomedical technology company, today released the results of research on the therapeutic potential of vagus nerve stimulation. In a paper published by Bioelectronic Medicine, Kevin J. Tracey, MD, and his colleagues at the Feinstein Institute, explore how low-level electrical stimulation interacts with the body’s nerves to reduce inflammation, a fundamental goal of bioelectronic medicine.
Prior to this study, it was not understood which vagus nerve fiber types were responsible for reducing the body’s inflammatory activity. The paper’s findings indicate that activation of either motor or sensory vagus nerve bundles can diminish inflammation.
“Identifying the exact role of the different nerve bundles in the inflammatory reflex bolsters our understanding of the relationship between the central nervous system and the vagus nerve,” said Dr. Kevin J. Tracey, president and CEO of the Feinstein Institute. “Furthermore, we now know that stimulating the vagus nerve for as little as half a millisecond is enough to inhibit tumor necrosis factor (TNF) production.”
After establishing the neural bundles activated in vagus nerve stimulation, the researchers found that only low-intensity, short-duration, electric pulses were needed to reduce the production of inflammation-inducing cytokines. Repetition of the pulses did not increase the success of the treatment in this experiment indicating that a single stimulating pulse is potentially sufficient.
“Seeing successful results with low-level electrical current is a significant finding,” said Yaakov Levine, PhD, senior research scientist, SetPoint Medical. “This indicates the potential for limited side effects, as well as promise for device miniaturization, both of which will be important to bringing vagus nerve stimulation into the mainstream.”
###
The findings of the paper represent another step forward for the field of bioelectronic medicine, a convergence of molecular medicine, bioengineering, and neuroscience. The emerging field aims to provide an alternative for treating a variety of diseases. SetPoint Medical has recently concluded a clinical trial using vagus nerve stimulation to treat rheumatoid arthritis and is currently exploring a similar treatment for Crohn’s disease. To read the paper in its entirety, visit bioelecmed.org.
About The Feinstein Institute for Medical Research
Headquartered in Manhasset, NY, The Feinstein Institute for Medical Research is home to international scientific leaders in many areas including Parkinson’s disease, Alzheimer’s disease, psychiatric disorders, rheumatoid arthritis, lupus, sepsis, human genetics, pulmonary hypertension, leukemia, neuroimmunology, and medicinal chemistry. The Feinstein Institute, part of the North Shore-LIJ Health System, ranks in the top 6th percentile of all National Institutes of Health grants awarded to research centers.
###
Emily Ng
[email protected]
516-562-2670
Profiling approach to enable right lung cancer treatment match

|
Manchester researchers have tested a new way to genetically profile lung cancer samples, potentially allowing doctors to more easily identify the most appropriate treatment for patients.
Non-small cell lung cancer (NSCLC) represents over 85% of lung cancer cases. The recent introduction of targeted therapies has led to improved patient survival, but only patients whose tumours have a specific genetic change are eligible for such treatments.
Identifying individual patients who may benefit from targeted therapy is becoming an essential part of treatment planning, but many current genetic analysis methods such as next generation sequencing require relatively large amounts of tumour material.
Dr Fiona Blackhall, a senior lecturer in The University of Manchester’s Institute of Cancer Sciences and a consultant based at The Christie NHS Foundation Trust - both part of the Manchester Cancer Research Centre - said: “Unfortunately the biopsy samples we take from these patients are generally quite small. In this study we looked at an alternative genetic screen that utilises a much smaller tissue biopsy to see if it can detect a range of changes in 26 key genes.”
The Lung Cancer research group working with the Manchester Centre for Genomic Medicine used the LungCarta platform to screen tumour samples from 90 NSCLC patients. They found that they could analyse over 95% of the samples and they detected genetic changes (mutations) that could be used for selection of treatment in around half of the biopsy samples.
“This type of genetic testing appears to be a clinically useful diagnostic screening test that can be used on small biopsy samples. This should allow us to better match lung cancer patients to the right treatment and we have now started to use this method of testing to identify suitable clinical trials for our patients,” added Dr Blackhall.
Jonathan Bernstein, a co-author on the paper, said: “Delivery and effectiveness of chemotherapy appears to be better in tumours with higher blood flow. However, amongst those patients with lower measured tumour blood flow, more work is needed to determine those who will and won’t respond.”
###
Jamie Brown
[email protected]
01-612-758-383
New method enables drug target validation for COPD treatment

|
Together with clinical partners, a team led by Dr. Dr. Melanie Königshoff and the doctoral student Franziska Uhl at the Comprehensive Pneumology Center of Helmholtz Zentrum München have investigated, for the first time, the suitability of Wnt/beta-catenin
activation to initiate repair in patient-derived COPD lung tissue. To achieve this, the researchers used a variety of chemical, biological and imaging techniques.
“In our study we showed that activation of the Wnt / beta-catenin ** - signaling pathway induces lung tissue repair, depending on the patient’s stage of COPD,” said Königshoff. The method developed by her team represents a powerful new tool for pathological assessment, drug validation, and mechanistic studies in patient-derived lung tissue, which will open novel avenues for successful clinical translation and precision medicine.
New method represents important advancement
“Previously, studies largely relied on animal models, and cell cultures in the petri dish were limited to two dimensions and individual time points,” said Uhl.
The new method makes it possible to visualize diseased lung tissue of patients and possible repair mechanisms in 3D with high spatio-temporal resolution, providing valuable insight into lung pathologies and suitable therapeutic avenues.
This method closes the gap that formerly existed between target identification and preclinical validation of drug compounds and their application in the patient. “We hope in this way to develop long-term treatments that induce lung tissue repair in the patients,” said Königshoff.
 Next, the research team plans to expand the study by increasing the patient cohort, and further optimize new treatment approaches for patients with COPD. Moreover, the team is currently extending the application to other lung diseases such as pulmonary fibrosis and lung cancer.
Next, the research team plans to expand the study by increasing the patient cohort, and further optimize new treatment approaches for patients with COPD. Moreover, the team is currently extending the application to other lung diseases such as pulmonary fibrosis and lung cancer.
###
Further information
Background:
*COPD stands for chronic obstructive pulmonary disease, a chronic inflammatory pulmonary disorder that leads to a narrowing of the smaller airways. It occurs primarily in smokers and is often accompanied by excessive mucus production and shortness of breath during exercise.
COPD is a chronic inflammatory lung disease. An estimated 13 percent of adults over 40 years in Germany suffer from it. The disease causes high economic losses. It is characterized by excessive mucus production and shortness of breath during exercise as well as a loss of functional lung tissue, the alveoli. At present, COPD cannot be cured; it is only possible to slow the disease progression. Lung transplantation is the only curative option, but this remains the exception due to the small number of donor organs.
**The Wnt signaling pathway is one of the many pathways for the transduction of signals through which the cells can react to external changes. The signaling pathway is named after its key player “Wnt”, a signaling protein that plays a major role as local mediator in the development of various animal cells. Numerous proteins are involved in the transduction of signals, including the beta-catenin protein.
Original Publikation
Preclinical validation and imaging of Wnt-induced repair in human 3D lung tissue cultures. DOI: 10.1183/09031936.00183214
###
Can cheap wine taste great? Brain imaging and marketing placebo effects

|
When consumers taste cheap wine and rate it highly because they believe it is expensive, is it because prejudice has blinded them to the actual taste, or has prejudice actually changed their brain function, causing them to experience the cheap wine in the same physical way as the expensive wine? Research in the Journal of Marketing Research has shown that preconceived beliefs may create a placebo effect so strong that the actual chemistry of the brain changes.
“Studies have shown that people enjoy identical products such as wine or chocolate more if they have a higher price tag,” write authors Hilke Plassmann (INSEAD) and Bernd Weber (University of Bonn). “However, almost no research has examined the neural and psychological processes required for such marketing placebo effects to occur.”
Participants in one of the studies were told they would consume five wines ($90, $45, $35, $10, $5) while their brains were scanned using an MRI. In reality, subjects consumed only three different wines with two different prices. Another experiment used labels to generate positive (“organic”) or negative (“light”) expectations of the pleasantness of a milkshake. Some consumed identical milkshakes but thought they would be either organic or regular; others consumed identical milkshakes but thought they would be either light or regular.
Participants showed significant effect of price and taste prejudices, both in how they rated the taste as well as in their measurable brain activity. The MRI readings related in part to specific areas of the brain that differ from person to person. These differences are also associated with known differences in personality traits. The authors were able to further determine that people who were strong reward-seekers or who were low in physical self-awareness were also more susceptible to having their experience shaped by prejudices about the product.
 “Understanding the underlying mechanisms of this placebo effect provides marketers with powerful tools. Marketing actions can change the very biological processes underlying a purchasing decision, making the effect very powerful indeed,” the authors conclude.
“Understanding the underlying mechanisms of this placebo effect provides marketers with powerful tools. Marketing actions can change the very biological processes underlying a purchasing decision, making the effect very powerful indeed,” the authors conclude.
###
Hilke Plassmann and Bernd Weber, “Individual Differences in Marketing Placebo Effects: Evidence from Brain Imaging and Behavioral Experiments.” Forthcoming in the Journal of Marketing Research. For more information, contact Hilke Plassmann or Mary-Ann Twist.
###
Mary-Ann Twist
[email protected]
608-255-5582
American Marketing Association
Journal
Journal of Marketing Research
Baclofen shows promise in patients with alcohol-induced liver disease

|
Results revealed today at The International Liver Congress™ 2015, show that in patients with alcohol-induced liver disease (ALD), Baclofen has a positive impact on alcohol consumption and overall measures of liver function and harm.
ALD is a major cause of alcohol-related mortality and helping patients with ALD to stop drinking is a primary goal of treatment. The primary aim of this study was to measure the effectiveness and tolerability of Baclofen in maintaining abstinence in this difficult to treat group, and to determine if this resulted in a reduction in standard measures of liver damage.
The results show promising outcomes for these patients, helping them to reduce their alcohol consumption as well as improving overall indicators of liver function and lowering physical dependence. A randomised controlled trial is now needed to confirm the benefit of Baclofen in this patient group.
###
About The International Liver Congress
This annual congress is the biggest event in the EASL calendar, attracting scientific and medical experts from around the world to learn about the latest in liver research.
Specialists share research studies and findings, and discuss the hottest topics related to liver disease. This year, the congress is expected to attract approximately 10,000 delegates from all corners of the globe. 2015 is a very special year for EASL and the hepatology community as they will celebrate the 50th annual meeting. The International Liver Congress™ takes place from April 22-26, 2015, Vienna, Austria.
About EASL
Since EASL’s foundation in 1966, this not-for-profit organisation has grown to over 4,000 members from more than 100 countries around the world. EASL is the leading liver association in Europe, it attracts the foremost hepatology experts and has an impressive track record in promoting research in liver disease, supporting wider education and promoting changes in European liver policy.
Contact
For more information, please contact the ILC Press Office at:
[email protected] or
+44 (0)20 3580 5444
###
EASL Press Office
[email protected]
Many European countries ill-prepared to prevent and control the spread of viral hepatitis

|
Many countries in the World Health Organization (WHO) European Region are facing limitations in conducting chronic viral hepatitis disease surveillance, assessing the burden of disease and measuring the impact of interventions, according to results revealed today at The International Liver Congress™ 2015.
The study highlights that less than one-third (27%) of WHO European Member States have national strategies in place that contain a surveillance component. Furthermore, only 64% have a national surveillance system for chronic hepatitis B and 61% for chronic hepatitis C.
The study also reveals the main areas in which governments would like the WHO’s support:
Development of national plans for viral hepatitis prevention and control (39%)
Estimation of the national burden of viral hepatitis (34%)
Surveillance (23%)
The results were obtained by analysing the responses to surveillance-related questions in the WHO Global Hepatitis Policy Survey. In total, 44 out of 53 (83%) of the WHO European Member States responded to the survey.
The study demonstrates a clear need for better disease surveillance and improvements in the development of national strategies to help prevent and control the spread of viral hepatitis in the WHO European region.
###
About The International Liver Congress
This annual congress is the biggest event in the EASL calendar, attracting scientific and medical experts from around the world to learn about the latest in liver research. Specialists share research studies and findings, and discuss the hottest topics related to liver disease. This year, the congress is expected to attract approximately 10,000 delegates from all corners of the globe. 2015 is a very special year for EASL and the hepatology community as they will celebrate the 50th annual meeting. The International Liver Congress™ takes place from April 22-26, 2015, Vienna, Austria.
About EASL
Since EASL’s foundation in 1966, this not-for-profit organisation has grown to over 4,000 members from more than 100 countries around the world. EASL is the leading liver association in Europe, it attracts the foremost hepatology experts and has an impressive track record in promoting research in liver disease, supporting wider education and promoting changes in European liver policy.
Contact
For more information, please contact the ILC Press Office at:
[email protected] or
+44 (0)20 3580 5444
What’s the life expectancy of patients when they begin treatment for osteoporosis?

|
Despite reports that people with osteoporosis have an increased risk of dying prematurely, a new study has found that life expectancy of newly diagnosed and treated osteoporosis patients is in excess of 15 years in women below the age of 75 and in men below the age of 60.
In more detailed analyses, the residual life expectancy after beginning osteoporosis treatment was estimated to be 18.2 years in a 50-year-old man and 7.5 years in a 75-year old man. Estimates in women were 26.4 years and 13.5 years. The Journal of Bone and Mineral Research study included 58,637 patients with osteoporosis and 225,084 age- and gender-matched controls. Information on deaths until the end of 2013 was retrieved, providing a follow-up period of 10 to 17 years.
“How best to treat patients with osteoporosis is a really simple issue when it comes to beginning treatment, but deciding how long to treat for is really very challenging,” said lead author Dr. Bo Abrahamsen. “The present study shows that most of the patients we treat have a long life expectancy. Therefore it is absolutely vital that we are not complacent but develop evidence-based strategies for the long-term management of osteoporosis.”
###
Dawn Peters
[email protected]
781-388-8408
Wiley
Journal
Journal of Bone & Mineral Research
Addressing the needs of young women with disorders of sex development

|
Disorders of sex development are lifelong conditions that are usually diagnosed at birth or during adolescence. In a recent study of 13 teenaged girls with disorders of sex development, the girls were guarded and reticent about sharing personal information about their disorder during adolescence, but some of them learned to engage in conversations with more confidence as they moved towards adulthood.
The participants noted that frustrations about their bodily differences and the limitations of their bodies limited physical spontaneity, impacted on their perceived sexual fulfillment, and hindered friendships or the possible formation of intimate partnerships. The young women wanted empathic, sensitive support from knowledgeable health professionals to help them understand their bodies.
“Our interpretive study aimed to provide professionals with insight into the experiences these young women faced in communicating aspects of their psychosocial development. We hope the wider audience recognizes the skills these young women may need as well as the scaffold of networks that can help them build and strengthen their social interactions,” said Dr. Caroline Sanders, lead author of the Journal of Advanced Nursing study.
###
Dawn Peters
[email protected]
781-388-8408
Wiley
Journal
Journal of Advanced Nursing
Total annual hospital costs could be reduced by rapid candidemia identification

|
A new study describes a model that estimates the economic consequences of using the T2Candida® Panel (a novel diagnostic product that provides Candida detection) as an adjunct to the current blood culture-based diagnostic strategy in a high-risk hospital patient cohort. It estimates that a typical hospital could save as much as $5,858,448 in total annual hospital costs. The study was published online ahead of print in Future Microbiology.
Candida species are a lethal form of common bloodstream infections that cause sepsis. They are associated with high patient mortality and excess inpatient costs because growth-based detection of Candida can delay treatment decisions. Improvements in outcomes are dependent on early identification of candidemia and timely administration of appropriate antifungal therapy. The T2Candida Panel is the first diagnostic test to provide species-specific Candida detection and identification directly from whole blood in 3 to 5 hours, without the need for blood culture.
“We are greatly encouraged by the benefits these data show for the early detection of Candida with our T2Candida Panel,” said John McDonough, chief executive officer of T2 Biosystems. “The findings from this study demonstrate not only significant reduction in hospital costs, but most importantly, the potential to save so many patient lives by providing faster diagnostic results - supporting our goal of changing the paradigm in sepsis diagnosis. We look forward to working closely with the medical community to help implement this important change.”
Using a decision tree model, the economic effect of using this diagnostic strategy over 1 year in a hospital setting was calculated. It also calculated Candida-related deaths per hospital could be reduced by 60.6%.
“Hospitals need to reduce the burden of bloodstream infections that cause sepsis in high risk patients, such as those with compromised immune systems. This new and interesting study estimates that that use of this diagnostic test could not only reduce hospital costs, but also reduce mortality rates,” said Natasha Leeson, Commissioning Editor of Future Microbiology.
 The article is freely available online at http://www.futuremedicine.com/doi/abs/10.2217/fmb.15.29 and will appear in an upcoming print edition of the journal.
The article is freely available online at http://www.futuremedicine.com/doi/abs/10.2217/fmb.15.29 and will appear in an upcoming print edition of the journal.
###
Notes for editors
About Future Microbiology
The journal publishes original research, reviews and opinion pieces that cover all aspects of microbiological sciences, including virology, bacteriology, parasitology and mycology. Essential information is delivered in concise, at-a-glance article formats. Key advances in the field are reported and analyzed by international experts, providing an authoritative but accessible forum for this increasingly important and vast area of research.
Future Microbiology has an impact factor of 3.819, which ranks it 27th by impact factor out of 119 journals in the Microbiology category. The journal is indexed by Biobase, BIOSIS Previews, BIOSIS Reviews Reports and Meetings, Biotechnology Citation Index®, CAB abstracts, Chemical Abstracts, EMBASE/Excerpta Medica, Journal Citation Reports/Science Edition®, MEDLINE/Index Medicus, Science Citation Index Expanded™ (SciSearch®) and Scopus.
To find out more about Future Microbiology, please visit our website: http://www.futuremedicine.com/loi/fmb
About Future Science Group
Founded in 2001, Future Science Group (FSG) is a progressive publisher focused on breakthrough medical, biotechnological and scientific research. FSG’s portfolio includes two imprints, Future Science and Future Medicine. Both publish eBooks and journals. In addition to this core publishing business FSG develops specialist eCommunities. Key titles and sites include Bioanalysis Zone, Epigenomics, Nanomedicine and the award-winning Regenerative Medicine.
The aim of FSG is to service the advancement of clinical practice and drug research by enhancing the efficiency of communications among clinicians, researchers and decision-makers, and by providing innovative solutions to their information needs. This is achieved through a customer-centric approach, use of new technologies, products that deliver value-for-money and uncompromisingly high standards. http://www.futuresciencegroup.com
###
Leela Ripton
[email protected]
44-208-371-6090
Future Science Group
Journal
Future Microbiology
UTMB develops new online tool for nurses

|
As tremendous advances are made in medicine, practitioners have new tools, but they also have more information to absorb and incorporate to provide evidence-based patient care: integrating best research evidence with clinical expertise and patient’s perspectives.
For the bedside nurse, this information can be lifesaving but time consuming. This has been a huge problem - until now.
The University of Texas Medical Branch has developed a new program that trains nurses how to pose questions that will point them to the needed information quickly. The Disciplined Clinical Inquiry - Evidence-Based Practice Literacy pathway is an online tool that helps nurses rapidly access filtered research evidence that present information in concise, easy to understand formats. An article describing this new program is available in the Journal for Nurses in Professional Development.
The EBP approach is becoming the “new normal” in patient care. UTMB’s online program offers a streamlined yet full education of the EBP skillset using online modules that take about three hours to learn. The standard DCI-EBP programs may take 50 hours to master.
“Mainstreaming EBP to bedside nurses with differing levels of professional experience, education, and generational profile is a challenge for nurses in professional development,” said Dolora Sanares-Carreon, lead author and EBP nursing program manager at UTMB. “There is a clear need for a simplified process for learning these skills in order to address the realities of patient care at the time of treatment.”
To ensure that the program was optimally designed, the researchers collected feedback from a focus group of nurses with various levels of practice and clinical specialties. Once completed, UTMB implemented the online program for all levels of nurses. The program has enhanced the ability of these nurses to engage in EBP.
 UTMB is hosting the second annual UTMB Health EBP National Conference on April 17-18, 2015 at the Galveston Island Convention Center. The goal of the 2015 conference is to examine real-world approaches to build and foster a transformative EBP health care ecosystem. Click here to register.
UTMB is hosting the second annual UTMB Health EBP National Conference on April 17-18, 2015 at the Galveston Island Convention Center. The goal of the 2015 conference is to examine real-world approaches to build and foster a transformative EBP health care ecosystem. Click here to register.
“DCI-EBP Literacy provides nurses with the tools they need to shift the focus from following protocols to a more dynamic approach focused on patient outcomes,” said Sanares-Carreon. “We are exploring a mobile app for nurses to use in addition to our online modules.”
###
The other authors of this paper include UTMB’s Odette Comeau, Diane Heliker, David Marshall, Charles Machner, Lynn Bell, Valerie Brumfield, Gail Kwarciany and Janet Sandridge.
###
Donna Ramirez
[email protected]
409-772-8791
University of Texas Medical Branch at Galveston
Journal
Journal for Nurses in Professional Development
Widespread agricultural contaminant impacts fish reproductive behavior

|
A common growth-promoting hormone used worldwide in the cattle industry has been found to affect the sexual behaviours of fish at a very low concentration in waterways - with potentially serious ecological and evolutionary consequences.
Researchers from Monash University, Australia in collaboration with researchers from Åbo Akademi University in Finland, have found that the steroid 17β-trenbolone - used on livestock to increase muscle growth - alters male reproductive behaviour in guppy fish (Poecilia reticulata).
This androgenic growth promoter is part of a group of contaminants called endocrine disrupting chemicals (EDCs) that enter the environment through a variety of sources - from discharge of household waste to agricultural run-off and industrial effluent.
Using trenbolone in livestock farming has been banned in the EU. However, in Denmark, researchers have measured high concentrations of it in gym sewage. Trenbolone is popular among bodybuilders. Trenbolone is used for example in the United States, Argentina and Australia.
One of the leading authors Dr Minna Saaristo, Academy of Finland Research Fellow in the Department of Biosciences at Åbo Akademi University, said over the past few decades concern has been mounting over EDCs, and that their contamination of aquatic habitats is a serious environmental problem.
“Endocrine disrupting chemicals (EDCs) are cause for concern given their capacity to disturb the natural functioning of the endocrine (hormonal) system, often at very low concentrations, with potentially catastrophic effects.
Research until now has focussed primarily on the morphological and physiological effects of EDC exposure. For the first time, our research has shown that exposure to an environmentally realistic concentration of 17β-trenbolone - just 22 nanograms per litre - is sufficient to alter male reproductive behaviour.”
The research shows that exposure of guppy fish to 17β-trenbolone influences the ratio of male courtship (where the female chooses her mate) to forced copulatory behaviour (sneaking), whereby the female is inseminated internally from behind and does not choose her mate. The results of her research indicated a marked increase in sneaking behaviour.
“By influencing mating success, sexual selection can profoundly affect individual populations and species, with potentially devastating long term evolutionary and ecological impacts”, Saaristo said.
With its widespread global distribution precipitated by numerous deliberate and accidental introductions, the small, live-bearing freshwater guppy fish, native to South America, was ideal for investigating the effects of 17β-trenbolone, especially as they are known to inhabit waterways receiving agricultural waste.
Saaristo said that by illustrating the capacity of the agricultural contaminant to alter reproductive behaviour, the research demonstrated the possibility of widespread disruption of mating systems in wild populations.
The next step for the researchers will be to look at sperm viability in male guppy fish exposed to 17β-trenbolone.
###
The research was published in the journal Hormones and Behavior, Volume 70, April 2015, Pages 85-91
More information:
Researcher at Åbo Akademi University
Dr. Minna Saaristo
E-mail: [email protected]
Phone: +61 (0) 406 747 713
Fat grafting technique improves results of breast augmentation

|
In women undergoing breast augmentation, a technique using transplantation of a small amount of the patient’s own fat cells can produce better cosmetic outcomes, reports a study in the April issue of Plastic and Reconstructive Surgery®, the official medical journal of the American Society of Plastic Surgeons (ASPS).
In particular, the fat grafting technique can achieve a more natural-appearing cleavage—avoiding the “separated breasts” appearance that can occur after breast augmentation, according to the report by Dr. Francisco G. Bravo of Clinica Gomez Bravo, Madrid.
Fat Grafting Adds to Cosmetic Results of Breast Augmentation
Dr Bravo analyzed the outcomes of breast augmentation surgery in 59 women. Thirty-eight women underwent conventional surgery using breast implants only. In the remaining 21 patients, Dr. Bravo used a combination technique using breast implants plus “selective para-sternal fat grafting.”
In this approach, a small amount of the patient’s own fat was harvested from elsewhere in the body - such as the thighs or abdomen. After processing, the fat cells were carefully placed along the inner (medial) borders of the breasts. The goal was to achieve a more natural shape, and particularly to soften the “medial transition zone” between the sternum (breastbone) and the implant edges.
Dr Bravo compared the results of women undergoing the two procedures by measuring the distance between the medial border of the breasts, or “vertical aesthetic line” (VAL). He also had 20 observers rate the attractiveness of paired breast photographs, digitally altered to show a narrower or wider VAL distance.
Both groups of women reported high satisfaction rates. However, the results showed a more natural cleavage in patients undergoing the fat grafting technique. As measured on postoperative photographs, the average VAL distance was 2.26 centimeters in women receiving implants only versus 0.6 centimeter with fat grafting plus implants.
On the breast attractiveness questionnaire, 95 percent of participants selected images with a narrower distance between breasts. There were no complications related to fat grafting—likely reflecting the small amounts of fat transplanted and the gentle “micro-grafting” technique used.
In recent years, several different fat grafting approaches have been evaluated for use in breast augmentation. Dr Bravo believes his combination technique may be especially useful in preventing the “separated breasts” deformity sometimes seen after implant-based breast augmentation. This problem is especially common in thin women, occurring when the edge of implant is visible on the inner side of the breast.
Careful fat grafting between the sternum and implant on both sides seems to provide a significant cosmetic advantage, producing a smoother transition between the breasts and avoiding the artificial “separated breasts” appearance. The results also support the concept that the VAL distance, as a measure of the space between breasts, is a useful concept for plastic surgeons to consider in achieving a more attractive, natural appearance after breast augmentation.
###
About Plastic and Reconstructive Surgery
For more than 60 years, Plastic and Reconstructive Surgery® (http://journals.lww.com/plasreconsurg/) has been the one consistently excellent reference for every specialist who uses plastic surgery techniques or works in conjunction with a plastic surgeon. The official journal of the American Society of Plastic Surgeons, Plastic and Reconstructive Surgery® brings subscribers up-to-the-minute reports on the latest techniques and follow-up for all areas of plastic and reconstructive surgery, including breast reconstruction, experimental studies, maxillofacial reconstruction, hand and microsurgery, burn repair, and cosmetic surgery, as well as news on medico-legal issues.
About ASPS
The American Society of Plastic Surgeons (ASPS) is the world’s largest organization of board-certified plastic surgeons. Representing more than 7,000 Member Surgeons, the Society is recognized as a leading authority and information source on aesthetic and reconstructive plastic surgery. ASPS comprises more than 94 percent of all board-certified plastic surgeons in the United States. Founded in 1931, the Society represents physicians certified by The American Board of Plastic Surgery or The Royal College of Physicians and Surgeons of Canada. ASPS advances quality care to plastic surgery patients by encouraging high standards of training, ethics, physician practice and research in plastic surgery.
Connie Hughes
[email protected]
646-674-6348
Germline TP53 mutations in patients with early-onset colorectal cancer

|
In a group of patients diagnosed with colorectal cancer at 40 or younger, 1.3 percent of the patients carried germline TP53 gene mutations, although none of the patients met the clinical criteria for an inherited cancer syndrome associated with higher lifetime risks of multiple cancers, according to a study published online by JAMA Oncology.
Li-Fraumeni syndrome is an inherited cancer syndrome usually characterized by germline TP53 mutations in which patients can develop early-onset cancers and have an increased risk for a wide array of other cancers including colorectal. The gene’s contribution to hereditary and early-onset colorectal cancer is needed for clinicians to counsel patients undergoing TP53 testing as part of a multigene risk assessment, according to the study background.
Sapna Syngal, M.D., M.P.H., of the Dana-Farber Cancer Institute, Boston, and coauthors estimated the proportion of patients with early-onset colorectal cancer who carry germline TP53 mutations. Participants were recruited from the Colon Cancer Family Registry from 1998 through 2007 and were those individuals who were diagnosed with colorectal cancer at 40 or younger and lacked a known hereditary cancer syndrome.
Among 457 eligible patients, six (1.3 percent) of them carried germline missense TP53 alterations and none of the patients met the clinical criteria for Li-Fraumeni syndrome, according to the results.
The authors note the fraction of patients found to carry germline TP53 mutations was comparable with the proportion of inherited colorectal cancer thought to be attributable to APC gene mutations.
“With modern techniques for comprehensively genotyping cancer patients, interpreting such germline results will undoubtedly be a prominent challenge in the counseling and management of at-risk individuals,” the study concludes.
###
 (JAMA Oncol. Published online March 12, 2015. doi:10.1001/jamaoncol.2015.0197. Available pre-embargo to the media at http://media.jamanetwork.com.)
(JAMA Oncol. Published online March 12, 2015. doi:10.1001/jamaoncol.2015.0197. Available pre-embargo to the media at http://media.jamanetwork.com.)
Editor’s Note: The authors made conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Media Advisory: To contact corresponding author Sapna Syngal, M.D., M.P.H., call Anne Doerr at 617-632-5665 or email [email protected].
###
Anne Doerr
[email protected]
617-632-5665
###
The JAMA Network Journals
Repairing the cerebral cortex: It can be done

|
A team led by Afsaneh Gaillard (Inserm Unit 1084, Experimental and Clinical Neurosciences Laboratory, University of Poitiers), in collaboration with the Institute of Interdisciplinary Research in Human and Molecular Biology (IRIBHM) in Brussels, has just taken an important step in the area of cell therapy: repairing the cerebral cortex of the adult mouse using a graft of cortical neurons derived from embryonic stem cells. These results have just been published in Neuron.
The cerebral cortex is one of the most complex structures in our brain. It is composed of about a hundred types of neurons organised into 6 layers and numerous distinct neuroanatomical and functional areas.
Brain injuries, whether caused by trauma or neurodegeneration, lead to cell death accompanied by considerable functional impairment. In order to overcome the limited ability of the neurons of the adult nervous system to regenerate spontaneously, cell replacement strategies employing embryonic tissue transplantation show attractive potential.
A major challenge in repairing the brain is obtaining cortical neurons from the appropriate layer and area in order to restore the damaged cortical pathways in a specific manner.
The results obtained by Afsaneh Gaillard’s team and that Pierre Vanderhaeghen at the Institute of Interdisciplinary Research in Human and Molecular Biology show, for the first time, using mice, that pluripotent stem cells differentiated into cortical neurons make it possible to reestablish damaged adult cortical circuits, both neuroanatomically and functionally.
These results also suggest that damaged circuits can be restored only by using neurons of the same type as the damaged area.
This study constitutes an important step in the development of cell therapy as applied to the cerebral cortex.
This approach is still at the experimental stage (laboratory mice only). Much research will be needed before there is any clinical application in humans. Nonetheless, for the researchers, “The success of our cell engineering experiments, which make it possible to produce nerve cells in a controlled and unlimited manner, and to transplant them, is a world first. These studies open up new approaches for repairing the damaged brain, particularly following stroke or brain trauma,” they explain.
###
This project was funded by the French National Research Agency (ANR-09-MNPS-027-01).
SOURCES
“Area-Specific Reestablishment of Damaged Circuits in the Adult Cerebral Cortex by Cortical Neurons Derived from Mouse Embryonic Stem Cells”
Kimmo A. Michelsen,1,2,5 Sandra Acosta-Verdugo,1,2,5,6 Marianne Benoit-Marand,3 Ira Espuny-Camacho,1,2 Nicolas Gaspard,1,2 Bhaskar Saha,3 Afsaneh Gaillard,3,*, and Pierre Vanderhaeghen1,2,4,*
1 Institut de Recherches en Biologie Humaine et Moléculaire (IRIBHM)
2 Neuroscience Institute, Université Libre de Bruxelles (ULB), Campus Erasme, 808 Route de Lennik, 1070 Brussels, Belgium
3 Unité Inserm1084, Experimental and Clinical Neurosciences Laboratory, Cellular Therapies in Brain Diseases Group, University of Poitiers,1 rue Georges Bonnet, BP 633, 86022 Poitiers Cedex, France
4 WELBIO, Université Libre de Bruxelles (ULB), Campus Erasme, 808 Route de Lennik, 1070 Brussels, Belgium
5 Co-first author
6 Present address: Department of Genetics, St. Jude Children’s Research Hospital, 262 Danny Thomas Place, Memphis, TN 38105, USA *Correspondence: [email protected] (A.G.), [email protected] (P.V.)
Neuron 85, 1-16, March 4, 2015
DOI: 10.1016/j.neuron.2015.02.001
RESEARCHER CONTACT
Afsaneh Gaillard
Head of “Cellular Therapies in Brain Diseases” research team, Inserm Joint Research Unit 1084, University of Poitiers
Tel.: + 33 (0)5 49 45 38 73
Email: [email protected]
###
Afsaneh Gaillard
[email protected]
###
INSERM (Institut national de la santé et de la recherche médicale)
Journal
Neuron
Clinical trial suggests combination therapy is best for low-grade brain tumors

|
New clinical-trial findings provide further evidence that combining chemotherapy with radiation therapy is the best treatment for people with a low-grade form of brain cancer. The findings come from a phase II study co-led by a researcher at Ohio State University Comprehensive Cancer Center - Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC - James) and researchers at the University of Maryland and at London Regional Cancer Program in Ontario, Canada.
The study shows that patients with low-grade gliomas and at high risk for tumor recurrence have an overall survival of 73 percent after three years when treated with radiation plus temozolomide, a chemotherapy drug. This is compared with a three-year survival of 54 percent for historical controls treated with radiation alone.
The findings are published in the International Journal of Radiation Oncology, Biology, Physics.
“The most effective treatment for these rare tumors is currently controversial at best,” says Arnab Chakravarti, MD, chair and professor of Radiation Oncology and co-director of the Brain Tumor Program at the OSUCCC - James. Chakravarti is the trial’s translational research national study chair.
“Many of these high-risk low-grade gliomas progress to grade III and IV tumors over time, so identifying the best treatment strategy is critical to ensure that patients have the best outcomes,” says Chakravarti, who is also the Max Morehouse Chair in Cancer Research at Ohio State.
“Our study reports that combining radiation with temozolomide-based chemotherapy appears to improve clinical outcome compared to historical controls treated by radiation alone. This may prove critical in killing enough tumor cells to prevent progression to stage IV disease, or glioblastoma multiforme, over time.”
Low-grade gliomas represent less than one percent of all human tumors in the United States. The average survival times vary depending on the tumor’s structural, molecular and genetic features. (One form of high-risk low-grade glioma has an average overall survival of about 5 years.)
The study’s key technical findings include:
The three-year progression-free survival rate was 59 percent.
Grade 3 adverse events occurred in 43 percent of patients; grade 4 events occurred in 10 percent of patients.
Chakravarti and his lab are currently conducting molecular studies to more specifically identify which low-grade glioma patients benefit from temozolomide.
###
Funding from the National Institutes of Health/National Cancer Institute (CA021661, CA037422, CA180868) supported this research.
Other researchers involved in this study were Barbara J. Fisher, MD, and David R. Macdonald, MD, London Regional Cancer Program, Ontario, Canada; Chen Hu, PhD, Radiation Therapy Oncology Group-Statistical Center, Philadelphia; Glenn J. Lesser, MD, Wake Forest University; Stephen W. Coons, MD, Barrow Neurological Institute, Phoenix; David G. Brachman, MD, Arizona Oncology Services Foundation, Phoenix; Samuel Ryu, MD, Henry Ford Hospital, Detroit; Maria Werner-Wasik, MD, Thomas Jefferson University, Philadelphia; Jean-Paul Bahary, MD, Centre Hospitalier de l’Universite´ de Montre´al-Notre Dame, Montreal, Quebec, Canada; Junfeng Liu, PhD, GCE Solutions, Inc., Bloomington, Illinois; Minesh Mehta, MD, University of Maryland.
The Ohio State University Comprehensive Cancer Center - Arthur G. James Cancer Hospital and Richard J. Solove Research Institute strives to create a cancer-free world by integrating scientific research with excellence in education and patient-centered care, a strategy that leads to better methods of prevention, detection and treatment. Ohio State is one of only 41 National Cancer Institute (NCI)-designated Comprehensive Cancer Centers and one of only four centers funded by the NCI to conduct both phase I and phase II clinical trials. The NCI recently rated Ohio State’s cancer program as “exceptional,” the highest rating given by NCI survey teams. As the cancer program’s 306-bed adult patient-care component, The James is a “Top Hospital” as named by the Leapfrog Group and one of the top cancer hospitals in the nation as ranked by U.S. News & World Report.
###
Darrell E. Ward
[email protected]
614-293-3737
###
Ohio State University Wexner Medical Center
Journal
International Journal of Radiation Oncology • Biology • Physics
Two-step treatment improved function and decreased pain severity in veterans

|
Although U.S. military veterans who have returned from Iraq or Afghanistan are more likely to suffer chronic pain than veterans of any other conflict in American history, little headway has been made in helping them manage the often debilitating effects of chronic pain. A new study by researchers from the Richard L. Roudebush VA Medical Center in Indianapolis, the Regenstrief Institute and the Indiana University School of Medicine reports that a stepped-care strategy improved function and decreased pain severity, producing at least a 30 percent improvement in pain-related disability.
“Pain is disabling and interferes with daily living as well as the ability to work,” said Matthew Bair, M.D., the VA and Regenstrief Institute investigator and IU associate professor of medicine who led the randomized controlled ESCAPE trial - short for Evaluation of Stepped Care for Chronic Pain. “It is a critical health issue among veterans, many of whom had multiple, often lengthy deployments.
“Many have significant long-term pain. We know that medications alone are only modestly successful in helping them; current pain treatments haven’t made much of a dent. The decrease in pain severity and 30 percent improvement in pain-related disability we achieved in the ESCAPE study are clinically significant, and we found that improvement lasted for at least nine months.”
Dr. Bair is an internist who treats veterans in primary care and is a health services researcher. Previously he served for eight years as a U.S. Army physician.
ESCAPE studied 241 veterans of Operations Enduring Freedom, Iraqi Freedom and New Dawn who suffer from musculoskeletal pain of the back, knee, neck or shoulder. Dr. Bair and colleagues developed a two-step program combining analgesics, self-management strategies and cognitive behavioral therapy.
The first step involved 12 weeks of medication treatment ranging from acetaminophen or naproxen sodium to opioids, coupled with pain self-management strategies such as deep breathing and other relaxation techniques. Step two involved 12 weeks of cognitive behavioral therapy drawing upon evidence-based psychological treatments for both pain and depression.
The ESCAPE program was provided over the telephone by nurse care managers. They worked with the veterans to help counter maladaptive thought and to help them better understand that while they might not be able to continue rigorous activities that they had enjoyed before deployment, a substitute activity like swimming might be achievable and decrease their pain.
Those who received the two-step ESCAPE program saw improvement in their function and a decrease in their pain severity and pain interference, or how pain interferes with mood, physical activity, work, social activity, relations with others, sleep and enjoyment of life.
Study patients randomized to usual care received educational handouts on musculoskeletal pain and were advised to discuss their pain with their physicians. These patients continued medications, clinic visits, specialty referrals and other care as usual.
All veterans in the study had suffered from moderate to severe chronic pain for more than three months. Veterans with current substance or alcohol dependence were excluded from the study, as were those with active suicidal ideation, active psychosis or schizophrenia. Two-thirds of the trial participants had served in the army, 88 percent were male, and 77 percent were white. The mean age was slightly under 37 years.
###
“Evaluation of Stepped Care for Chronic Pain (ESCAPE) in Veterans of Iraq and Afghanistan Conflicts: A Randomized Trial” appears in the March 9 issue of JAMA Internal Medicine.
Authors in addition to Dr. Bair are Dennis Ang, M.D., of Wake Forest School of Medicine; Jingwei Wu, M.S., Christy Sargent, B.S., and Zhangsheng Yu, Ph.D., of IU School of Medicine; Carol Kempf, R.N., Amanda Froman, B.S., and Louanne W. Davis, Psy.D., of the Roudebush VA Medical Center; Arlene A. Schmid, Ph.D., OTR, of Colorado State University; and Samantha D. Outcalt, Ph.D., Teresa M. Damush, Ph.D., and Kurt Kroenke, M.D., of the Richard L. Roudebush VA Medical Center, the Regenstrief Institute and IU School of Medicine.
According to the authors, ESCAPE challenges existing treatment paradigms for chronic pain. They report that patients randomized to the innovative two-step approach spoke of an evolving understanding of their pain experience during the trial, and of how this new understanding helped them manage their pain more effectively.
The ESCAPE study was supported by a grant from VA Rehabilitation Research & Development. The views expressed in the study are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
###
Cindy Fox Aisen
[email protected]
317-843-2276
Indiana University
Journal
JAMA Internal Medicine
Online health information - keep it simple!

|
Australian health websites are too difficult for many people to read.
This is the finding from a study published in Australian and New Zealand Journal of Public Health.
Matthew Dunn and Christina Cheng from Deakin University evaluated Australian online health information to see if it matched the reading level of Australians.
“Limited availability of ‘easy-to-read’ health materials suggests that many Australians may not be benefiting from the convenience of the internet,” Dr Dunn said.
“For example, more than 12 million Australians were overweight or obese in 2007, yet the 17 web pages found that formally discussed obesity were among the hardest to read.”
If information is difficult to read, many readers may misinterpret it, leading to inappropriate healthcare decisions.
 About 16 million Australians are active online and almost 80% of them seek out health information on the internet.
About 16 million Australians are active online and almost 80% of them seek out health information on the internet.
“Reading habits on the web are different from reading printed information. Web users tend to skim a page before deciding to read further, which can leave important information unread,” Dr Dunn said.
“The flexible and interactive nature of the internet has provided health professionals with a tool to increase knowledge of health matters in the population.
“Websites need to be assessed for readability and changes need to be made so that a larger proportion of the population can understand their information.”
###
The Australian and New Zealand Journal of Public Health is published by the Public Health Association of Australia. Information on the Association and the Journal can be found at http://www.phaa.net.au
###
Dr. Matthew Dunn
[email protected]
61-352-278-372
Wiley
Journal
Australian and New Zealand Journal of Public Health
Quitting smoking has favorable metabolic effects

|
People who quit smoking have improved metabolic effects, a new study finds. The results will be presented in a poster Thursday, March 5, at ENDO 2015, the annual meeting of the Endocrine Society in San Diego.
“In general, people think that when they stop smoking, they are going to gain weight and their diabetes and insulin resistance are going to get worse, but we didn’t find that,” said principal investigator Theodore C. Friedman, MS, MD, PhD, chair of the Department of Internal Medicine of Charles R. Drew University of Medicine and Science in Los Angeles, California. “Our study showed that insulin resistance was basically the same and some of the fat redistribution seemed to be better. Initially fat might have gone into the abdomen, but later, it went back to the thigh, which is more benign.”
In this study, researchers enrolled healthy, ½-to-2 pack-per-day smokers into an 8-week smoking cessation program of behavioral counseling plus oral bupropion (Phase I), followed by a 16-week maintenance period without counseling or bupropion wherein subjects either remained abstinent or naturally resumed/increased smoking (Phase II).
Before and after Phase 1, the researchers measured the subjects’ number of cigarettes per day, breath carbon monoxide, urine nicotine metabolites, weight, body composition, fat distribution, free fatty acids, and rate of glucose release from the liver and overall glucose utilization.
Study results showed that smoking cessation over 8 weeks was associated with a slight and transient worsening of central fat distribution, followed by a larger, favorable reversal over subsequent months. Over 24 weeks, hepatic glucose output improved in relation to lifestyle changes, weight change correlated directly with reduced nicotine metabolites, and reduced carbon monoxide and/or nicotine metabolites correlated with increased glucose uptake and utilization of carbohydrate substrates as the preferred metabolic fuel.
“Smoking cessation appears to have complex but generally favorable metabolic effects, and they should be encouraged. Cessation also seems to lead to beneficial effects in terms of where the fat is and what happens with hepatic glucose release from the liver,” he said.
###
The California Tobacco-Related Diseases Research Program (TRDRP) (administered by Friends Research Institute, Inc.), NIH CDU Diversity-Promoting Institutions Drug Abuse Research Development Program (DIDARP), the American Diabetes Association Clinical-Translational Research Grant, the Accelerating Excellence in Translational Science (AXIS); and the UCLA Clinical and Translational Science Institute (CTSI) supported this study.
###
Aaron Lohr
[email protected]
202-971-3654
The Endocrine Society
Meeting
ENDO 2015: The 97th Annual Meeting & EXPO in San Diego, CA
Garlic extract could help cystic fibrosis patients fight infection
|
|
A chemical found in garlic can kill bacteria that cause life-threatening lung infections in people with cystic fibrosis, research suggests.
The study is the first to show that the chemical - known as allicin - could be an effective treatment against a group of infectious bacteria that is highly resistant to most antibiotics.
Allicin is produced naturally by garlic bulbs to ward off a closely-related group of plant pathogens found in soil and water habitats. In the 1980s, the bacteria - known as the Burkholderia cepacia complex (Bcc) - emerged as a cause of serious and transmissible lung infections in people with cystic fibrosis.
Measures to limit the spread of Bcc infections among people with cystic fibrosis have brought the number of cases down considerably. However, current therapies available to treat infections - that are potentially fatal - are limited and require the use of combinations of three to four antibiotics at a time.
Researchers found that allicin - which can be extracted by crushing raw garlic - inhibits the growth of bacteria and, at higher doses, kills the plant pathogens. The team suggests that allicin kills Bcc bacteria by chemically modifying key enzymes. This deactivates them and halts important biological processes within the pathogens’ cells.
The team believes allicin-containing remedies could be used in combination with existing antibiotics to treat Bcc infections. However, the researchers say it is important to pinpoint the mechanisms by which allicin kills the bacteria before the chemical can be incorporated into new treatments.
The Bcc are highly versatile plant and human pathogens that have not been studied to the same extent as other superbugs - such as MRSA - the team says.
The bacteria produce potent antimicrobial agents which kill bacteria and fungi, making them naturally drug-resistant and allowing them to survive in polluted and antibiotic-rich environments.
The team says the Bcc also have a range of potential uses in the agriculture industry.
The study, published in the journal PLoS One, was funded by the University of Edinburgh and the Biotechnology and Biological Sciences Research Council.
Professor John Govan, of the University of Edinburgh’s Centre for Infectious Diseases, who co-led the study, said: “At a time when novel antimicrobial agents are urgently required, chemical and microbiological research has the potential to unlock the rich reservoir of antimicrobial compounds present in plants such as garlic. Allicin-containing compounds merit further investigation as adjuncts to existing treatments for infections caused by Bcc.”
Dr Dominic Campopiano, of the University of Edinburgh’s School of Chemistry, said: “The medicinal power of garlic has a rich history that dates back thousands of years but the chemical structure of allicin was only revealed in the 1940s. Our work suggests that modern methods should be used to further expand our knowledge of this enigmatic molecule and rejuvenate its potential applications.”
###
Corin Campbell
[email protected]
44-131-650-6382
University of Edinburgh
Journal
PLOS ONE
Your privacy online: Health information at serious risk of abuse

|
There is a significant risk to your privacy whenever you visit a health-related web page. An analysis of over 80,000 such web pages shows that nine out of ten visits result in personal health information being leaked to third parties, including online advertisers and data brokers.
This puts users are risk for two significant reasons: first, people’s health interests may be publicly identified along with their names. This could happen because criminals get ahold of the information, it is accidentally leaked, or data brokers collect and sell the information. Second, many online marketers use algorithmic tools which automatically cluster people into groups with names like “target” and “waste”. Predictably, those in the “target” category are extended favorable discounts at retailers and advance notice of sales. Given that 62 percent of bankruptcies are the result of medical expenses, it is possible anyone visiting medical websites may be grouped into the “waste” category and denied favorable offers.
For individuals, this means profiles are built based on web page visits, potentially resulting in someone being labeled a commercial risk due to the fact that they have used a site like WebMD.com or CDC.gov to look up health information for themselves, a family member, or a friend. Given that data brokers are free to sell any information they collect regarding visits to health websites, those visiting such sites are potentially at risk of being discriminated against by potential employers, retailers, or anybody else with the money to buy the data.
These findings are reported in the article “Privacy Implications of Health Information Seeking on the Web,” appearing in the March 2015 issue of Communication of the ACM.
Timothy Libert, a doctoral student at the University of Pennsylvania’s Annenberg School for Communication wrote the article. He authored a software tool that investigates Hypertext Transfer Protocol (HTTP) requests initiated to third party advertisers and data brokers. He found that 91 percent of health-related web pages initiate HTTP requests to third-parties. Seventy percent of these requests include information about specific symptoms, treatment, or diseases (AIDS, Cancer, etc.). The vast majority of these requests go to a handful of online advertisers: Google collects user information from 78 percent of pages, comScore 38 percent, and Facebook 31 percent. Two data brokers, Experian and Acxiom, were also found on thousands of pages.
“Google offers a number of services which collect detailed personal information such as a user’s persona email (Gmail), work email (Apps for Business), and physical location (Google Maps),” Libert writes. “For those who use Google’s social media offering, Google+, a real name is forcefully encouraged. By combining the many types of information held by Google services, it would be fairly trivial for the company to match real identities to “anonymous” web browsing data.” Indeed, in 2014, the The Office of the Privacy Commissioner of Canada found Google to be violating privacy Canadian laws.
“Advertisers promise their methods are wholly anonymous and therefore benign,” Libert writes. “Yet identification is now always required for discriminatory behavior to occur.” He cites a 2013 study where individuals’ names were associated with web searches of a criminal record, simply based on whether someone had a “black name.”
“Personal health information - historically protected by the Hippocratic Oath - has suddenly become the property of private corporations who may sell it to the highest bidder or accidentally misuse it to discriminate against the ill,” Libert said. “As health information seeking has moved online, the privacy of a doctor’s office has been traded in for the silent intrusion of behavioral tracking.”
Online privacy has for some time been a concern. Studies conducted by Annenberg dating back to 1999 indicate wariness among Americans about how their personal information may be used. And slightly more than one in every three Americans even knows that private third-parties can track their visits to health-related websites.
Libert points out that the Federal Health Insurance Portability and Accountability Act (HIPPA) is not meant to police business practices by third party commercial entities or data brokers. The field of regulation is widely nonexistent in the U.S., meaning that individuals looking up health information online are left exposed and vulnerable.
According to Libert, “Proving privacy harms is always a difficult task. However, this study demonstrates that data on online health information seeking is being collected by entities not subject to regulation oversight. This information can be inadvertently misused, sold, or even stolen. Clearly there is a need for discussion with respect to legislation, policies, and oversight to address health privacy in the age of the internet”.
###
Joseph J. Diorio
[email protected]
215-746-1798
###
University of Pennsylvania Annenberg School for Communication
Journal
Communications of the ACM
UW research shows sensor technology may help improve accuracy of clinical breast exams

|
Sensor technology has the potential to significantly improve the teaching of proper technique for clinical breast exams (CBE), according to a new study by researchers at the University of Wisconsin School of Medicine and Public Health.
The results of the study were published in a correspondence today in the New England Journal of Medicine.
Carla Pugh, director of patient safety and education at the University of Wisconsin Hospital and Clinics and principal investigator of the study, says the use of sensors allows a level of critical analysis unavailable to clinicians until recently.
“Variations in palpable force used during a CBE cannot be reliably measured by human observation alone,” Pugh says. “Our findings revealed that 15 percent of the physicians we tested were using a technique that put them at significant risk of missing deep tissue lesions near the chest wall. This research underscores the potential for sensor technology to be used not only to improve clinical performance, but to also allow for objective evidence-based training, assessment and credentialing.”
For the study, Pugh and her team asked 553 practicing physicians during annual clinical meetings of the American Society of Breast Surgeons, American Academy of Family Physicians and American College of Obstetricians to perform simulated CBE under conditions that mimic an office visit for a symptomatic patient. Participants completed a demographic survey, reviewed a clinical scenario, performed the CBE on a sensor-enabled breast model, and then documented their findings. The goal was to capture CBE technique while clinicians were purposefully seeking a mass.
The sensor data revealed that physicians who palpated fewer than 10 newtons (a common measurement of force) were able to find two superficial masses on the breast model but missed the two deeper ones. The physicians who increased the amount of palpation pressure improved the probability that they would identify the deeper lesions. The study suggests that the optimal palpable force for deeper lesions is between 12 and 17 newtons.
“I want to spark a serious conversation about the potential for high-end, mastery training in the health care profession,” Pugh says. “Health care is at a critical juncture where there are huge opportunities for major information exchanges that can empower physicians and patients. Both patients and physicians will benefit from clinical-skills performance data.”
In 2011, Pugh received the Presidential Early Career Award for Scientists and Engineers (PECASE) for her research on the sensor device used in the study. Other researchers on this project include Shlomi Laufer, a research fellow in Pugh’s lab, and Anne-Lise D’Angelo, a resident in the division of general surgery at the UW Hospitals and Clinics and a graduate student in educational psychology at UW-Madison.
###
The study was funded by a grant from the National Institutes of Health (RO1EB011524).
###
Gian Galassi
[email protected]
608-263-5561
###
University of Wisconsin-Madison
Journal
New England Journal of Medicine
Joslin researchers find drugs are effective for diabetic macular edema in new trial
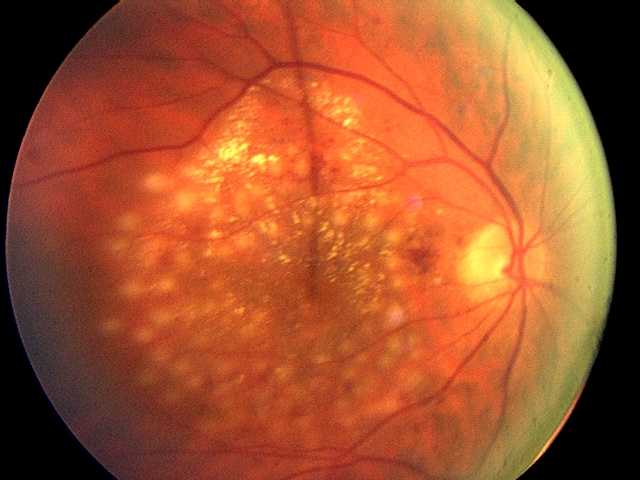
|
In the first clinical trial directly comparing three drugs most commonly used to treat diabetic macular edema, researchers found all were effective in improving vision and preventing vision loss. However, one drug, aflibercept, provided greater improvement for people with more severe vision loss when treatment was initiated. The trial was conducted by the National Eye Institute Diabetic Retinopathy Clinical Research Network (DRCR.net) including researchers from Joslin Diabetes Center. The results appeared in the February online edition of the New England Journal of Medicine.
Diabetes is a significant risk factor for developing eye diseases. The most common diabetic eye disease and a leading cause of blindness is diabetic retinopathy, which is caused by elevated blood sugar levels damaging the blood vessels of the retina and affects approximately 7.7 million Americans. About 750,000 Americans with diabetic retinopathy have diabetic macular edema (DME) in which fluid leaks into the macula, the area of the retina used when looking straight ahead. The fluid causes the macula to swell, blurring vision. “DME is the leading cause of moderate vision loss in working-age adults with diabetes. With the rate of diabetes increasing dramatically worldwide, many individuals will be at risk for vision loss from diabetic eye complications and DME is a major global health concern,” says Jennifer K. Sun, M.D., M.P.H., a member of the study research team and writing committee, and an Investigator in the Section on Vascular Biology, an ophthalmologist in Beetham Eye Institute at Joslin and an Assistant Professor at Harvard Medical School.
In an earlier study, Joslin researchers reported that VEGF, a major growth factor for blood vessels, is elevated in the eye fluids of patients with proliferative diabetic retinopathy and DME, causing leakage and the growth of abnormal blood vessels.
Over the past few years, drugs that target VEGF have become a standard treatment for DME, providing a preferred alternative or adjunct to laser treatment. The standard Medicare per-injection costs of the three anti-VEGF drugs evaluated in the study are about $1960 for aflibercept (Eylea), $1200 for ranibizumab (Lucentis) and $70 for bevacizumab (Avastin).
At the start of the trial, 660 adults with DME were enrolled: their average age was 61 years and 90 percent had type 2 diabetes. About half of the participants had 20/32 or 20/40 vision and the other half had vision of 20/50 or worse. They were randomized into three treatment groups and received the assigned study drug by injection into the eye until the DME resolved or stabilized. Participants on bevacizumab and ranibizumab received, on average, 10 injections, versus nine for those on aflibercept.
One year after starting treatment, all participants had improved vision. Those with mild vision loss (20/32 to 20/40) at baseline in all three treatment groups gained on average almost two lines on an eye chart. For participants with more severe vision loss (20/50 or worse), aflibercept improved vision on average nearly four lines, bevacizumab about 2.5 lines, and ranibizumab almost three lines.
“The results clearly remove any doubts about anti-VEGF drugs’ efficacy in treating DME. All three drugs improved vision substantially, with aflibercept showing more visual gains in patients with worse vision at the start of the trial. Physicians now have robust data to help them counsel patients and make informed decisions regarding treatment options,” says study co-author Lloyd P. Aiello, M.D., Ph.D., Professor of Ophthalmology at Harvard Medical School, Director of Joslin’s Beetham Eye Institute, co-head of Joslin’s Section of Vascular Cell Biology, and founding chair of the DRCR Network.
In light of these positive results, “it is more important than ever for patients with diabetes to be evaluated on a regular basis for eye disease and receive treatment promptly once indicated as we now have excellent success in treating patients with DME,” says Dr. Aiello.
###
The trial was supported through a cooperative agreement from the National Eye Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, U.S. Department of Health and Human Services. Regeneron Pharmaceutical provided the aflibercept and Genentech provided the ranibizumab for the study. The DRCR.net had complete control over the design of the study, data ownership and content of presentations and publications related to this study.
About Joslin Diabetes Center
Joslin Diabetes Center, based in Boston, Massachusetts, undertakes diabetes research, clinical care, education and health and wellness programs on a global scale. Joslin is dedicated to ensuring that people with diabetes live long, healthy lives and offers real progress in preventing and curing diabetes. Joslin is an independent, nonprofit institution affiliated with Harvard Medical School, and is recognized worldwide for driving innovative solutions in diabetes prevention, research, education, and care.
Our mission is to prevent, treat and cure diabetes. Our vision is a world free of diabetes and its complications. For more information, visit http://www.joslin.org.
About Joslin Research
Joslin Research comprises the most comprehensive and productive effort in diabetes research under one roof anywhere in the world. With 30-plus faculty-level investigators, Joslin researchers focus on unraveling the biological, biochemical and genetic processes that underlie the development of type 1 and type 2 diabetes and related complications.
Joslin research is highly innovative and imaginative, employing the newest tools in genetics, genomics and proteomics to identify abnormalities that may play a role in the development of diabetes and its complications. Joslin Clinic patients, and others with diabetes, have the option of participating in clinical trials at Joslin to help translate basic research into treatment innovations.
Joslin has one of the largest diabetes training programs in the world, educating 150 M.D. and Ph.D. researchers each year, many of whom go on to head diabetes initiatives at leading institutions all over the globe.
###
Jeff Bright
[email protected]
###
Joslin Diabetes Center
Journal
New England Journal of Medicine
Drug improves measures of genetic disease that affects liver, spleen

|
Among previously untreated adults with Gaucher disease type 1, a genetic disease in which there is improper metabolism due to a defect in an enzyme, treatment with the drug eliglustat resulted in significant improvements in liver and spleen size hemoglobin level, and platelet count, according to a study in the February 17 issue of JAMA.
Gaucher disease type 1 is characterized by enlargement of the spleen and liver, anemia, low blood platelets, chronic bone pain, and the failure to grow properly. Untreated Gaucher disease type 1 is a chronic and progressive disorder associated with disability, reduced life expectancy, and, in some patients, life-threatening complications. The current standard of care is enzyme replacement therapy, which requires lifelong intravenous infusions every other week. A safe, effective oral therapy is needed, according to background information in the article.
Pramod K. Mistry, M.D., Ph.D., F.R.C.P., of the Yale University School of Medicine, New Haven, Conn., and colleagues randomly assigned 40 untreated adults with Gaucher disease type 1 to receive eliglustat (twice daily; n = 20) or placebo (n = 20) for 9 months. Eliglustat is a novel oral medication, which showed favorable results for patients with this disease in a phase 2 trial. This phase 3 trial was conducted at 18 sites in 12 countries.
The researchers found that administration of eliglustat resulted in a reduction in spleen volume of approximately 30 percent compared with placebo, as well as improvements in hemoglobin level, decreased liver volume (-6.6 percent), and increased platelet count (41 percent). No serious adverse events occurred. No patient discontinued treatment over the course of the 9-month study because of a treatment-emergent adverse event.
Gaucher disease is a rare genetic disorder in which a person lacks an enzyme called glucocerebrosidase.
Alternative Names
Glucocerebrosidase deficiency; Glucosylceramidase deficiency
Gaucher disease affects an estimated 1 in 50,000 to 1 in 100,000 people in the general population. Persons of Eastern and Central European (Ashkenazi) Jewish heritage are more likely to get this disease.
It is an autosomal recessive disease. This means that the mother and father must both pass one abnormal copy of the gene to the child in order for the child to develop the disease. A parent who silently carries an abnormal copy of the gene is called a carrier.
The lack of the glucocerebrosidase enzyme causes harmful substances to build up in the liver, spleen, bones, and bone marrow. The substances prevent cells and organs from working properly.
There are three main subtypes of Gaucher disease:
Type 1 disease is most common. It involves bone disease, anemia, an enlarged spleen and thrombocytopenia. Type I affects both children and adults. It is most common in the Ashkenazi Jewish population.
Type 2 disease usually begins in infancy with severe neurologic involvement. This form can lead to rapid, early death.
Type 3 disease may cause liver, spleen, and brain problems. Patients may live into adulthood.
 The authors add that more definitive conclusions about clinical efficacy and utility will require comparison with the standard treatment of enzyme replacement therapy as well as longer-term follow-up.
The authors add that more definitive conclusions about clinical efficacy and utility will require comparison with the standard treatment of enzyme replacement therapy as well as longer-term follow-up.
###
(doi:10.1001/jama.2015.459; Available pre-embargo to the media at http://media.jamanetwork.com)
Editor’s Note: This trial was funded by Genzyme. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, etc.
###
Ziba Kashef
[email protected]
###
The JAMA Network Journals
Journal
JAMA
HPV vaccination not associated with increase in sexually transmitted infections

|
A barrier to human papillomavirus (HPV) vaccination has been the concern that it may promote unsafe sexual activity, but a new study of adolescent girls finds that HPV vaccination was not associated with increases in sexually transmitted infections (STIs), according to an article published online by JAMA Internal Medicine.
Nearly one-quarter of U.S. females between the ages 14 and 19 and 45 percent of women between the ages of 20 and 24 are affected by HPV. The HPV vaccination can prevent cervical, vulvar and vaginal cancers and genital warts caused by certain HPV strains. Still, HPV vaccination rates remain low in the United States and, by 2013, only 57 percent of females between the ages of 13 and 17 had received at least one dose, whereas only 38 percent had received all three recommended doses, according to the study background.
Anupam B. Jena, M.D., Ph.D., of Harvard Medical School, Boston, and coauthors used a large insurance database of females (ages 12 to 18) from 2005 through 2010 to examine STIs among girls who were vaccinated and those who were not.
The authors found use of the vaccination increased over time with 27.3 percent of females receiving the vaccination by the end of 2010 compared with just 2.5 percent of females at the end of 2006. The study included 21,610 females who were vaccinated against HPV and 186,501 matched females who were nonvaccinated.
The study found that females who were vaccinated were more likely to be sexually active in the year before vaccination compared with those who were nonvaccinated. Study results also indicate that vaccinated females had higher rates of STIs before and after vaccination compared with those who were nonvaccinated. For example, the rates of STIs in the year before vaccination were higher among HPV-vaccinated females (94 of 21,610, 4.3 per 1,000) compared with nonvaccinated females (522 of 186,501, 2.8 per 1,000). The rates of STIs increased both for vaccinated (147 of 21,610, 6.8 per 1,000) and nonvaccinated (781 of 186,501, 4.2 per 1,000) girls in the year after vaccination. The difference in odds between the two groups implies that the HPV vaccination was not associated with an increase in STIs relative to the growth of STIs among nonvaccinated females.
“We found no evidence that HPV vaccination leads to higher rates of STIs. Given low rates of HPV vaccination among adolescent females in the United States, our findings should be reassuring to physicians, parents and policy makers that HPV vaccination is unlikely to promote unsafe sexual activity,” the study concludes.
(JAMA Intern Med. Published online February 9, 2015. doi:10.1001/jamainternmed.2014.7886. Available pre-embargo to the media at http://media.jamanetwork.com.)
Editor’s Note: This study was funded by a grant from the National Institutes of Health and a grant from the National Institute of Aging. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Commentary: HPV and Sexual Activity, Addressing Parent, Physician Concerns
In a related commentary, Robert A. Bednarczyk, Ph.D., of Emory University, Atlanta, writes: “However, just as we do not wait until we have been in the sun for two hours to apply sunscreen, we should not wait until after an individual is sexually active to attempt to prevent HPV infection.”
“The hesitancy on the part of parents and physicians to vaccinate or discuss vaccination may be attributable to worries that HPV vaccination will be seen as a tacit approval for sexual activity. ... In this issue of JAMA Internal Medicine, Jena et al add to the literature by presenting a novel analysis that indicates no evidence for increased sexual activity after HPV vaccination,” he continues.
“These findings should not come as a surprise to researchers in the field of HPV vaccinology and should serve as continued reassurance that HPV vaccination does not lead to sexual disinhibition. However, this reassurance leaves us with the question, “How can we use these findings to address concerns of anxious parents of adolescents? ... To date, much research has been conducted to identify HPV vaccination barriers, but less research has been conducted to identify the preferred content and mode of delivery of information to mitigate these barriers. Addressing this knowledge gap through the development and delivery of information relative to all key partners (adolescents, their parents and their health care professionals) will be critical in removing the stigma of HPV vaccine in our efforts to fully use this vaccine,” Bednarczyk concludes.
(JAMA Intern Med. Published online February 9, 2015. doi:10.1001/jamainternmed.2014.7894. Available pre-embargo to the media at http://media.jamanetwork.com.)
Editor’s Note: The author made conflict of interest disclosures. The commentary was supported in part by a grant from the National Institutes of Health. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
###
Media Advisory: To contact author Anupam B. Jena, M.D., Ph.D., call David Cameron at 617-432-0441 or email [email protected]. To contact commentary author Robert A. Bednarczyk, Ph.D., call Melva Robertson at 404-727-5692 or email [email protected].
###
David Cameron
[email protected]
617-432-0441
###
The JAMA Network Journals
Journal
JAMA Internal Medicine
Study identifies 8 signs associated with impending death in cancer patients

|
Researchers at The University of Texas MD Anderson Cancer Center have identified eight highly specific physical and cognitive signs associated with imminent death in cancer patients. The findings, published in the journal Cancer, could offer clinicians the ability to better communicate with patients and families. They may also guide both the medical team and caregivers on complex decision making, such as discontinuation of tests and therapy, plans for hospital discharge and hospice referral.
Previous studies in end-of-life care have focused on physicians prognosticating better. However, according to David Hui, M.D., assistant professor, Palliative Care and Rehabilitation Medicine, research on how to tell if a patient has entered the final days of life has been minimal. Knowing with a high degree of confidence that death is imminent could have significant implications for clinical practice. It may also help families and caregivers make more informed decisions.
“In the past, studies trying to understand the signs associated with impending death were conducted in people who were recognized as dying, so there’s a potential bias built into this model. With our study, we observed a list of signs in patients from the time they were admitted to the palliative care unit. They were observed systematically, twice a day, without knowing if the patient would die or be discharged,” says Hui, the study’s corresponding author.
The study shows that very simple observations by doctors and care teams can help make a very important diagnosis and may inform both the patient and the family so that they can make difficult personal decisions, he explained.
For the prospective study, Hui and colleagues at MD Anderson and Barretos Cancer Hospital (an MD Anderson Sister Institution in Brazil) observed 357 cancer patients admitted to the respective palliative care units, of which 57 percent ultimately died. The researchers systematically observed 52 physical and cognitive signs - identified by Hui and colleagues in previous research - twice a day from the patient’s admission to discharge or death. Of those 52 signs, the researchers identified the eight most highly associated with impending death within three days. Signs include: nonreactive pupils; decreased response to verbal stimuli; decreased response to visual stimuli; inability to close eyelids; drooping of the nasolabial fold; neck hyperextension; grunting of vocal cords; and upper gastrointestinal bleeding.
 “When cancer patients reach the last days of life, this is an extremely emotional time for families - their stress levels cannot be understated,” says Hui. “Knowing when death is imminent would provide more information so caregivers can plan appropriately. For clinicians, having this information could help reassure families that we are providing the best care possible.”
“When cancer patients reach the last days of life, this is an extremely emotional time for families - their stress levels cannot be understated,” says Hui. “Knowing when death is imminent would provide more information so caregivers can plan appropriately. For clinicians, having this information could help reassure families that we are providing the best care possible.”
Hui stresses that this research is not yet practice-changing, but is an important step in understanding these eight signs and their relation to impending death. Also, says Hui, the findings are only representative of imminent cancer death and should not be generalized to other causes of death.
Follow up studies in different settings are planned: Hui and colleagues will look at the reliability of the identified signs, as well as evaluate this research in other countries and in the hospice setting.
###
In addition to Hui, other authors on the study include: from MD Anderson, Eduardo Bruera, M.D., professor and chair, and Swati Bansal, both of Palliative Care and Rehabilitation Medicine; and Gary Chisholm, Biostatistics. From Barretos Cancer Hospital, authors include: Renata dos Santos, M.D., and Camila Souza Crovador.
###
Laura Sussman
[email protected]
713-745-2457
University of Texas M. D. Anderson Cancer Center
Journal
Cancer
BGI study confirms accuracy of its NIFTY in nearly 147,000 pregnancies

|
BGI has published a study tracking the clinical performance of its whole genome sequencing-based non-invasive prenatal test (the NIFTY® test) in nearly 147,000 pregnancies, the largest such study to date. The results showed high sensitivity and specificity and no significant difference between high-risk and low-risk pregnant women.
The study, published in the journal Ultrasound Obstetrics and Gynecology, reported on 146,958 samples from 508 medical centers in mainland China, which were collected between early 2012 and mid-2013 for trisomy 21, 18, and 13. Although NIFTY® measures other chromosomal abnormalities, these results were not included in the study.
According to the study’s results, NIFTY® identified 1,578 trisomy-positive and 145,380 negative samples. Comparing the results with follow-up confirmatory invasive testing, or by tracking patients’ eventual pregnancy outcomes, the study team then calculated the false positive (FPR) and false negative rate (FNR) for each tested trisomy, and the overall sensitivity, specificity, and positive predictive value (PPV).
Overall, the study showed the sensitivity of NIFTY® as 99.1 percent, 98.2 percent, and 100 percent in the three trisomies (T21, T18, T13), respectively. Specificity was 99.95 percent in each case. For T21, the FPR was 0.05 percent, and the PPV was 92.19 percent. For T18, the FPR was also 0.05 percent, and the PPV was 76.6 percent. FPR and PPV for T13 were 0.04 percent and 32.84 percent, respectively.
The study confirms the performance metrics of earlier smaller studies of NIPT from both NIFTY® and other providers, in a significantly expanded sample range. The data also shows that the NIFTY® test’s performance did not differ substantially among higher- and lower-risk women.
Wang Wei, the study’s first author, comments, “In this paper, we showed the first-hand information of NIPT performance in a very large population, and consistency with the accuracy shown in small studies. The results also suggested that high quality of NIPT service can be achieved at NGS-based clinical labs with strict protocols and standards.”
Importantly, the study authors note that most confirmed false positives and false negatives in the study could be traced to noticeable biological factors, such as maternal copy number variation or mosaicism. Wang said that the group was somewhat surprised to find that low fetal fraction was not a major contributor to NIPT misdiagnoses in their cohort, considering that the importance of fetal fraction has been “overwhelmingly emphasized in the past few years, and low fetal fraction is believed to be a major risk of causing NIPT false results.”
With the largest and most comprehensive evidence of NIPT performance in low-risk pregnant women, Wang expects “a bright future of using NIPT in the general population.”
###
Press Office
[email protected]
BGI Shenzhen
Journal
Ultrasound Obstetrics and Gynecology
Hepatitis C more prevalent than HIV/AIDS or Ebola yet lacks equal attention

|
More than 180 million people in the world have hepatitis C, compared with the 34 million with HIV/AIDS and the roughly 30,000 who have had Ebola. Yet very little is heard about the hepatitis C virus (HCV) in the way of awareness campaigns, research funding or celebrity fundraisers.
One of the global regions highly affected by hepatitis C is West Africa. In developed countries, hepatitis C, a blood-borne disease, is transmitted through intravenous (IV) drug use. “In West Africa, we believe that there are many transmission modes and they are not through IV drug use, but through cultural and every day practices,” says Jennifer Layden, MD, PhD principal investigator on a study recently published in the journal Clinical Infectious Diseases. “In this study, tribal scarring, home birthing and traditional as opposed to hospital based circumcision procedures, were associated with hepatitis C infection in Ghana.”
The study was conducted by HepNet, an international multidisciplinary group of physicians and scientists. “The other important finding was that a high percentage of individuals who tested positive for HCV had evidence of active infection,” says Layden. “This illustrates the need for treatment.”
Discovering the source of the disease and a target population, she says, will aid in the next step of the research: how to protect and prevent the disease in Ghana.
Dr. Layden and colleagues from Loyola’s Department of Public Health Sciences organized the inaugural HepNet meeting Aug. 12 and 13, 2013, in Kumasi, Ghana. Loyola University is the lead investigator in the HepNet research, with collaboration from the Komfo Anokye Teaching Hospital in Ghana, the Centers for Disease Control and the Johns Hopkins University. This is the first published research study from the HepNet group.
“This is a small study conducted at a blood bank in a teaching hospital in Ghana,” says Layden. “We have now expanded studies to test more than 5,000 individuals in Ghana.” The goal is to further understand whom is affected by hepatitis C and to identify specific next steps in intervention and prevention.
“Hep C is a chronic disease and leads to chronic liver disease, liver cancer and cirrhosis,” says Layden. “Overall, worldwide rates of liver cancer is on the rise, whereas many other cancers are on the decline or steady.” Layden says the study offers hope for West Africa.
Similar studies have been conducted in Egypt, a country with high rates of hepatitis C infection.
“Those studies helped to call attention to the widespread infection rate and resulted in getting infected Egyptians affordable medical treatment,” says Layden. “We in HepNet hope our studies will do the same in Ghana and other West African countries.”
###
Participating researchers from Loyola University Chicago, Stritch School of Medicine,
Maywood, Illinois are: Jennifer Layden; Stephanie Kliethermes; Nallely Mora; Lara Dugas; Amy Luke; David Shoham and Richard S. Cooper.
###
Stasia Thompson
[email protected]
708-216-5155
###
Loyola University Health System
Journal
Clinical Infectious Diseases
Physician guidelines for Googling patients need revisions

|
With the Internet and social media becoming woven into the modern medical practice, Penn State College of Medicine researchers contend that professional medical societies must update or amend their Internet guidelines to address when it is ethical to “Google” a patient. “As time goes on, Googling patients is going to become more and more common, especially with doctors who grew up with the Internet,” says Maria J. Baker, associate professor of medicine. Baker has dealt with the question first hand in her role as a genetic counselor and medical geneticist. In a case that inspired her recent paper in the Journal of General Internal Medicine, a patient consulted her regarding prophylactic mastectomies. The patient’s family history of cancer could not be verified and then a pathology report revealed that a melanoma the patient listed had actually been a non-cancerous, shape-changing mole.
Turning to the Internet, Baker found evidence of the patient capitalizing on being a cancer victim for a cancer she did not have. The question, Baker says, is in what circumstances is it appropriate for a doctor to research a patient using online search engines? “Googling a patient can undermine the trust between a patient and his or her provider, but in some cases it might be ethically justified,” Baker says. “Healthcare providers need guidance on when they should do it and how they should deal with what they learn.”
With regard to future guidelines, Baker and her co-authors suggest 10 situations that may justify patient-targeted Googling:
Duty to re-contact/warn patient of possible harm
Evidence of doctor shopping - visiting different doctors until a desired outcome is acquired.
Evasive responses to logical clinical questions
Claims in a patient’s personal or family history that seem improbable
Discrepancies between a patient’s verbal history and clinical documentation
Levels of urgency/aggressiveness are not justified by clinical assessment
Receipt of discrediting information from other reliable health professionals that calls the patient’s story into question
Inconsistent statements by the patient, or between a patient and their family members
Suspicions regarding physical and/or substance abuse
Concerns regarding suicide risk
“Under certain circumstances - when carefully thought out - it may be appropriate to Google a patient,” said Baker. “We’re hoping that by offering scenarios that raise important ethical questions about the use of search engine technology, we can initiate a conversation that results in the eventual development of professional guidelines. What are the justifications? How is this information that you might potentially learn going to impact the patient-provider relationship and how are you going to document the information about the patient that you might learn?”
Formal professional guidelines could help healthcare providers navigate this current “Google blind spot,” said Baker. While professional medical groups such as the American Medical Association and the Federation of State Medical Boards provide general guidance on appropriate Internet and social media use, they have yet to address patient-targeted Web searches.
“Any professional medical society’s policy statements on the use of the Internet and social media - which they should all have - should undergo revision to help provide guidance to their various health care providers,” Baker says.
###
Co-authors on this paper are Daniel R. George, assistant professor of medical humanities, and Gordon L. Kauffman, professor and vice chair of surgery, both at Penn State College of Medicine.
###
Matt Solovey
[email protected]
717-531-8606
###
Penn State
Journal
Journal of General Internal Medicine
How negative stereotyping affects older people

|
The most comprehensive analysis to date of research on the effect of negative stereotypes on older people’s abilities has concluded that these stereotypes create a significant problem for that demographic.
A research team at the University of Kent’s School of Psychology carried out a review and meta-analysis of Aged-Based Stereotype Threat (ABST).
They statistically analysed international evidence from 37 research studies, both published and unpublished. They concluded that older adults’ memory and cognitive performance is negatively affected in situations that signal or remind them of negative age stereotypes. These effects affect both men and women.
The research, funded by the Economic and Social Research council (ESRC), was carried out by Ruth Lamont, working with Dr Hannah Swift and Professor Dominic Abrams. It further found that older people’s cognitive performance suffers more when the threat is induced by stereotypes rather than by facts.
The meta-analysis showed that even a hint that performance was being pre-judged because of age criteria was enough to affect older people’s performance.
Ruth Lamont said that the study evidence highlighted that even ‘subtle differences’ in the way people behave toward older people - such as being patronising or speaking slowly - could be enough to make them underperform when others are testing their abilities, either formally or informally.
Researchers have previously concluded that stereotype threat affects the major social categories of gender and ethnicity, but this new meta-analysis, which looked at evidence from over a decade of research, highlights the need to be just as concerned about age stereotypes, Ruth Lamont suggested.
The research team further conclude that the vulnerability of some older adults to ABST when they perform memory, cognitive or physical tasks has important social, economic and clinical implications which will become more relevant given an increasingly aging population and workforce.
###
The paper, titled A Review and Meta-Analysis of Age-Based Stereotype Threat: Negative Stereotypes, Not Facts, Do the Damage, is published in the American Psychological Association’s journal Psychology and Ageing.
###
Martin Herrema
[email protected]
01-227-823-581
###
Journal
Psychology and Ageing
Researchers identify efficient methylating enzyme for cancer development
|
A recent study may help begin to explain how cancer develops though the abnormal turning on and off of genes. Researchers have discovered that the increase of methyl tags in cancer cells is due to highly efficient DNA methyl transferase 1 (DNMT1) enzymes found in these cells. The findings appear in the Journal of Proteomics and Bioinformatics.
Both plants and animals have genetic machinery that modifies the information and function of their genomes without actually changing their genetic code. This modification process is known as “epigenetics.” One of the best studied of these epigenetic processes involves the chemical tagging of DNA nucleotides across the genome using methyl groups. These “methyl tags” are attached to cytosine nucleotides in specific patterns around genes and other expressed sequences by a specialized group of enzymes called methyltransferases.
Genes that are expressed and turned into proteins are free of “methyl” tags, but when such methyl tags attach to DNA, gene expression is turned off. “Whether methyl tags are added to genes varies during normal development and during the development of diseases like cancer, and understanding these processes is currently a major topic of research,” explained corresponding author Sibaji Sarkar, PhD, instructor of medicine at Boston University School of Medicine (BUSM). According to Sarkar it was previously discovered that cancer cells have more methyl tags than normal cells and level of the enzyme which adds the tag, DNA methyl transferase1 (DNMT1) is also higher, but no one knew that both increases are not proportional.
The researchers focused on two types of cells - cancer cells and normal healthy cells. For each cell type, they used mathematical Hill equation to determine whether the methylation status (methyl tags present as compared to those which were absent) of eight selected genes correlated with the amount of DNA methyl transferase1 (DNMT1) enzyme present in the cells. They found that the enzyme that adds these tags (DNMT1) worked more efficiently in genes which are silenced in cancer cells as compared with normal healthy cells. Interestingly, the enzyme did not work efficiently with the genes which are not silenced by methylation in cancer cells. This increase in enzyme activity is called allostericity and it is observed in many cellular processes including addition of oxygen to hemoglobin to carry oxygen efficiently. The outstanding mystery which remains to be solved is, how this enzyme selectively chooses some genes to efficiently methylate.
“Since this highly efficient DNMT1 enzyme can promote cancer development, using a drug that inhibits this allosteric increase in enzyme activity may someday be beneficial for cancer treatment, because it will target the super active methylation process in cancer cells. We are developing a combination therapy that uses this type of epigenetic drugs in combination with other more traditional drugs, and researchers have shown that such treatments are effective and able to reduce cancer relapse,” he said. The idea behind the addition of epigenetic drugs in combination therapy is to make cancer cells susceptible and possibly kill cancer progenitor cells and drug resistance cancer cells.
Sarkar and his colleagues believe these findings begin to clarify how the regulation of DNMT1 impacts the normal and abnormal addition of methyl tags, and thus, gene transcription in general. “Hopefully, through this and future work, we will discover the molecular mechanisms that lead to differential silencing and expression of genes during human development from embryogenesis and the aberration of this process in many diseases including cancer development. This knowledge will hopefully develop methods of counteracting these mechanisms and treating cancer,” he added. The discovery that DNMT1 efficiently methylate selective genes brings us one step closer to the idea of “on” and “off” switch of cancer development. Recent studies have shown that genes are transcriptionally silenced by the creation of an insulated area, which regulate enhancer and transcription factor interactions. The formation and deformation of these areas in development and disease conditions including cancer possibly are regulated by this highly efficient methylation mechanism.
###
Also contributing to this study were first author Eric Samorodnitsky, PhD from Ohio State University, Boston University student Emily Ghosh and Sahana Mazumder, PhD from Rammohan College, University of Kolkata.
Partial funding of Sarkar’s laboratory work was provided by a grant from the American Cancer Society.
###
Gina DiGravio
[email protected]
617-638-8480
Boston University Medical Center
Journal
Journal of Proteomics and Bioinformatics
Funder
American Cancer Society
Gene may open door for improved keloid, scar treatment
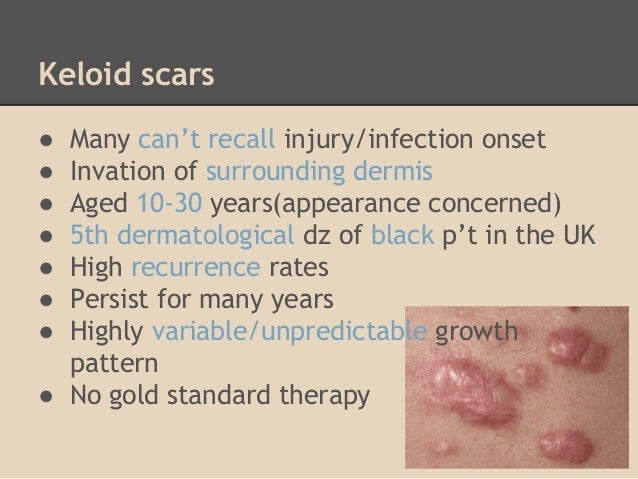
|
Researchers at Henry Ford Hospital in Detroit have identified a gene that may offer a better understanding of how keloid scars develop and potentially open the door to improved treatment for the often painful, itchy and tender scars.
The study is the first to demonstrate that an altered AHNAK gene may have a significant biological role in keloid development.
“This finding has great promise for better understanding how keloids function and offer a potential target for improved and novel treatments,” says study lead author Lamont R. Jones, M.D., Vice Chair, Department of Otolaryngology-Head and Neck Surgery at Henry Ford.
“We now have a better understanding of how this gene fits in the broader picture of the wound healing process, which may be important in preventing scars in general.”
Study results will be presented today, Jan. 23, at the 2015 Triological Combined Sections Meeting in San Diego.
Keloid scars form raised, firm skin areas and most often occur on the chest, shoulders, earlobes (following ear piercing), upper arms and cheeks. Unlike regular scars, keloids do not subside over time and often extend outside the wound site.
The lowest rates of keloid formation have been documented in albinos and the highest seen in dark skinned individuals, especially in the African-American population.
When skin is injured, fibrous tissue (called scar tissue) forms over the wound to repair and protect the injury. In some cases, scar tissue grows excessively, forming smooth, hard growths called keloids. Keloids can be much larger than the original wound, and are most commonly found on the upper chest and shoulders. However, keloids can affect any part of the body. (NZDSI)
Although keloids are not harmful to your health, they may present cosmetic concerns.
What Symptoms Are Associated with Keloids?
Keloids occur from the overgrowth of scar tissue; symptoms will occur at a site of previous skin injury.
Symptoms include:
area that is flesh-colored, pink or red in color
a lumpy or ridged area of skin
an area that continues to grow larger with scar tissue over time
itchy patch of skin
Keloid scars tend to be larger than the original wound itself. They may take weeks or months to fully develop.
While keloid scars may be itchy, they are typically not harmful to your health. You may experience some discomfort or tenderness, or possible irritation from clothing or other forms of friction. In rare instances, a person may experience keloid scarring on a significant amount of their body. When this occurs, the hardened, tight scar tissue may restrict your movements.
Keloids are often more of a cosmetic concern than a health one. You may feel self-conscious if the keloid is very large or in a highly visible location, such as an earlobe or on the face. Sun exposure or tanning may discolor the scar tissue, making it slightly darker than your surrounding skin. This can make the keloid stand out even more than it already does. Keep the scar covered when you are in the sun to prevent discoloration.
Treatment for keloids includes cortisone injections, pressure dressings, silicone gels, surgery, cryosurgery (freezing), laser treatment, or radiation therapy. A combination of treatments may be used, depending on the individual. In some cases, keloids return after treatment, up to 50 to 100 percent of the time.
AHNAK is a 700 kDa protein located on the cell membrane in epithelial cells and in the nucleus and cytoplasm of other cell types such as fibroblasts. AHNAK has been suspected to contribute to cell-cell adhesion or exocytosis.
 For their study, Dr. Jones and his colleges investigated AHNAK as a potential biomarker in keloids through the integration of methylation and gene expression.
For their study, Dr. Jones and his colleges investigated AHNAK as a potential biomarker in keloids through the integration of methylation and gene expression.
To do so, the Henry Ford team examined samples of fresh keloid tissue and fresh normal tissue for AHNAK expression.
Three of the five keloid samples showed a large reduction in expression as compared to the normal tissue.
What are keloid scars?
Collagen gathers around the damage and builds up to help the wound seal over. The resulting scar usually fades over time, becoming smoother and less noticeable.
However, some scars don’t stop growing. They “invade” the surrounding healthy skin and become bigger than the original wound. These are known as keloid scars.
Some scars become red and raised within the size of the original wound. These are called hypertrophic scars. Find out more about hypertrophic scars.
“A keloid scar is an overgrown scar that can spread outside the original area of skin damage,” says Hermione Lawson of the British Skin Foundation. “Keloid scars are shiny and hairless, they’re raised above the surrounding skin, and can feel hard and rubbery.”
Keloids affect around 10-15% of all wounds. They can appear anywhere on the body, but usually form on the shoulders, head and neck.
They can last for years and sometimes don’t form until months or years after the initial injury. New keloid scars are sometimes red or purple. They’re not usually painful, but some people feel embarrassed or upset if they think the scar is disfiguring them.
Experts don’t fully understand why keloid scarring happens, but these scars are not contagious (they’re not catching) and there is no risk of them turning into cancer.
In this small sample, gene expression was consistent with methylation, a process that allows the researchers to look for genetic abnormalities within tumor samples.
“Identifying AHNAK puts our translational research one step closer to moving from the bench to the bedside,” says Dr. Jones.
###
In addition to Dr. Jones, study co-authors from Henry Ford are Joshua Greene, M.D.; Kang Mei Chen, M.D.; George Divine, Ph.D.; Dhananjay Chitale, M.D.; Veena Shah, M.D.; and Maria J. Worsham, Ph.D.
###
Krista Hopson Boyer
[email protected]
313-874-7207
Henry Ford Health System
Dislocating a hip after total hip replacement can be a traumatic experience

|
Osteoarthritis of the hip is a degenerative joint disease that, besides being painful, also has a negative impact on mobility. An affected joint can be surgically replaced with an artificial prosthesis to alleviate pain and enhance mobility and quality of life. However, when the replacement hip is forced from its normal position-a so-called dislocation-these patients frequently experience injuries, undermining their trust in the artificial joint. Depending on the trauma that caused the dislocation, it may even be necessary to replace the prosthesis. In their current review article published in Deutsches Ärzteblatt International (Dtsch Arztebl Int 2014; 111: 884-90), Jens Dargel et al. point out that the prevention of dislocation plays an important role and describe the risks that need to be addressed.
Approximately 1 in 50 patients who undergo total hip replacement for the first time will experience a dislocation. Among patients with total hip replacements that required revision and implant exchange surgeries, this rate can be as high as 1 in 4 patients (up to 28%). Here the risks include advanced age and concomitant neurological conditions.
Moreover, patients should make sure to avoid certain movements, such as bending too far forward, as these can increase the risk for dislocation of the implant. Further risks arise at the time the surgery is performed: incorrect positioning of the implant, inadequate soft-tissue tension and inadequate experience of the surgeon all add to the risk for dislocation. The authors recommend using a standardized approach for the management of dislocation following total hip replacement, based on a diagnostic and therapeutic algorithm.
###
SUMMARY
Background: Hip replacement ranks among the more successful operations on
the musculoskeletal system, but it can have serious complications. A common
one is dislocation of the total hip endoprosthesis, an event that arises in about
2% of patients within 1 year of the operation. Physicians should be aware of
how this problem can be prevented and, if necessary, treated, so that the
degree of trauma due to hip dislocation after hip replacement surgery can be
kept to a minimum.
Methods: The authors searched Medline selectively for pertinent publications
and analyzed the annual reports of international endoprosthesis registries.
Results: The rate of dislocation of primary hip replacements ranges from 0.2%
to 10% per year, while that of artificial hip joints that have already been surgi-
cally revised can be as high as 28%, depending on the patient population, the
follow-up interval, and the type of prosthesis. Patient-specific risk factors for
displacement of a hip endoprosthesis include advanced age, accompanying
neurologic disease, and impaired compliance. Patients should scrupulously
avoid hip movements such as bending far forward from a standing position, or
internal rotation of the flexed hip. Operation-specific risk factors include
suboptimal implant position, insufficient soft-tissue tension, and inadequate
experience of the surgeon. Conservative treatment is justified the first time
dislocation occurs without any identifiable cause. If a mechanical cause of
instability is found, then operative revision should be performed as recom-
mended in a standardized treatment algorithm, because, otherwise, dislocation
is likely to recur.
Conclusions: The dislocation of a total hip endoprosthesis is an emotionally
traumatizing event that should be prevented if possible. Preoperative risk
assessment should be performed and the operation should be performed with
optimal technique, including the best possible physical configuration of implant
components, soft-tissue balance, and an adequately experienced orthopedic
surgeon.
Jens Dargel
[email protected]
Deutsches Aerzteblatt International
Journal -
Deutsches Ärzteblatt International
SPECTAcolor viable next generation multinational cancer clinical trial infrastructure

|
SPECTAcolor’s successful start has demonstrated its viability to facilitate next generation cancer clinical trials. It has been successfully implemented across 19 clinical centers located in nine countries in Europe, has now recruited over 500 patients since its launch in September 2013, and the observed frequency of mutations is similar to that observed in previous colorectal cancer clinical trials. In addition, pathological review and core analyses of tumor blocks shipped to the central biobank at Dresden University Hospital for central quality deemed over 98% of the samples were adequate. This successful implementation is evidence that a logistically complex infrastructure to run next generation trials in a multinational setting is feasible.
These results were presented by SPECTAcolor coordinator Dr. Gunnar Folprecht of the Dresden University Hospital at the 2015 Gastrointestinal Cancers Symposium held 15-17 January 2015 in San Francisco.
J Clin Oncol 33, 2015 (suppl 3; abstr 575)
Treatments for patients with cancer are becoming more and more tailored to the molecular characteristics of the particular patient and disease. Consequently, molecularly characterizing a patient’s disease is now a prerequisite for them to access the appropriate clinical trial for their particular cancer. Assessing their tumor, however, is more easily said than done, because the required testing is beyond the scope of most hospitals. Cancer is too diverse, so the EORTC built a collaborative molecular screening platform, SPECTAcolor, which provides the necessary infrastructure to screen adult patients with advanced stage colorectal cancer for mutations in colorectal cancer biomarkers.
A preliminary analysis of biological materials from 293 patients for five baseline cancer biomarkers showed:
KRAS was wild type for exon 2, 3 and 4 in 151 patients and mutated in 133 patients (114 patients in exon 2, 8 patients in exon 3, and 11 patients in exon 4);
NRAS was tested in KRAS wild type patients only and mutations were found in 14 patients (6 patients in exon 2 and 8 patients in exon 3);
BRAF mutations, all in exon 15, were found in 18 patients;
PI3K mutations occurred in 41 patients (13 in exon 20 and 28 in exon 9);
IHC staining was showing deficient mismatch repair in 16 patients.
Tumor samples are also being analyzed by Next Generation Sequencing for 360 key cancer genes in cooperation with the Sanger Institute (Cambridge, UK).
###
SPECTAcolor provides an excellent opportunity for molecular oriented clinical trials in Europe based on innovative and high quality partnership models with pharmaceutical industry and is supported by a unique partnership between the EORTC Charitable Trust and the Corporate Social Responsibility Program of Alliance Boots.
###
John Bean
[email protected]
Journal of Clinical Oncology
Study suggests increase in falls among the elderly

|
Over a 12-year period, the prevalence of self-reported falls among older adults appeared to be on the rise, according to a new nationally representative study.
Falling is the most frequent cause of injury among older adults and about a third of older adults fall each year. Researchers analyzed data from 1998-2010 among adults age 65 and over and found an 8 percent increase in falls - which translates to a relative increase of nearly 30 percent.
The findings appear in JAMA Internal Medicine.
“We expected an increase because older adults are getting older and there are more 80 and 90 year old adults than before, but we were very surprised to find that the increase in falls was not due to the changing demography,” says lead author Christine Cigolle, M.D., M.P.H., assistant professor in the departments of Family Medicine and Internal Medicine at the University of Michigan and a research scientist at the VA Ann Arbor Healthcare System Geriatric Research, Education and Clinical Center (GRECC).
“We saw a higher number of falls across all age groups - not just the oldest -and that was unexpected.”
Researchers looked at trends in falling in a nationally representative sample of middle-aged and older adults in the Health and Retirement Study, which is conducted by the U-M Institute for Social Research on behalf of the National Institute of Aging.
Falling was defined as at least one self-reported fall in the preceding two years. Among all adults 65 and older, the two-year prevalence of self-reported falls increased from about 28 % in 1998 to 36 % in 2010.
HOW OFTEN FALLS OCCUR
About one third of the elder population over the age of 65 falls each year, and the risk of falls increases proportionately with age. At 80 years, over half of seniors fall annually.
As alarming as they are, these documented statistics fall short of the actual number since many incidents are unreported by seniors and unrecognized by family members or caregivers.
Frequent falling. Those who fall are two to three times more likely to fall again.
About half (53%) of the older adults who are discharged for fall-related hip fractures will experience another fall with in six months
Falls are the leading cause of death due to injury among the elderly 87% of all fractures in the elderly are due to falls.
Falls account for 25% of all hospital admissions, and 40% of all nursing home admissions 40% of those admitted do not return to independent living; 25% die within a year.
Many falls do not result in injuries, yet a large percentage of non-injured fallers (47%) cannot get up without assistance.
For the elderly who fall and are unable to get up on their own, the period of time spent immobile often affects their health outcome. Muscle cell breakdown starts to occur within 30-60 minutes of compression due to falling. Dehydration, pressure sores, hypothermia, and pneumonia are other complications that may result.
Getting help after an immobilizing fall improves the chance of survival by 80% and increases the likelihood of a return to independent living.
Up to 40% of people who have a stroke have a serious fall within the next year.
Despite the greater prevalence of reported falls, however, the study did not find that older adults were reporting more fall injuries.
Authors note that programs like “Matter of Balance” that focus on making older adults more aware of balance and provide strategies to reduce risks of falling, may also improve reporting. However, further research is needed to identify possible reasons behind the numbers, such as an increase in fall risk factors (e.g., cardiovascular and psychiatric medications that may have side effects like dizziness) or an increase in fall risk behavior.
“It’s possible that older adults are more aware of fall risk and may be more likely to report it now than before,” says Cigolle, who is also a member of the Institute of Gerontology and the Institute for Healthcare Policy and Innovation. “However, if the prevalence of falls is actually increasing as much as it seems to be, we need to do more work to identify possible factors and how we can address what we know to be a high risk among a vulnerable group.”
###
U-M is among 10 clinical trial sites in the country for a major study on preventing fall injuries among the elderly and to find effective, evidence-based strategies to address the personal and public health burden of falls. The trial is funded by the National Institutes of Health and the Patient-Centered Outcomes Research Institute (PCORI). GRECC Director Neil Alexander, M.D., M.S., professor in the Division of Geriatrics and Palliative Medicine at the U-M Medical School, is the lead investigator for the U-M site.
Additional Authors: Jinkyung Ha, Ph.D.; Lillian Min, M.D., MSHS; Pearl G. Lee, M.D. M.S; Neil Alexander, M.D. M.S., all of U-M. Caroline Blaum, M.D., M.S., formerly of U-M and now with New York University Langone Medical Center. Tanya Gure M.D., of Ohio State University Wexner Medical Center.
Funding: Dr. Cigolle is supported by grant K08 AG031837 from the National Institute on Aging.
Reference: “More older Americans report falling: the epidemiology of falls, 1998-2010,” JAMA Intern Med., Jan.19, 2015, doi:10.1001/jamainternmed.2014.7533.
###
Beata Mostafavi
[email protected]
734-764-2220
University of Michigan Health System
Cell-associated HIV mucosal transmission: The neglected pathway

|
Dr. Deborah Anderson from Boston University School of Medicine (BUSM) and her colleagues are challenging dogma about the transmission of the human immunodeficiency virus type 1 (HIV-1). Most research has focused on infection by free viral particles, while this group proposes that HIV is also transmitted by infected cells. While inside cells, HIV is protected from antibodies and other antiviral factors, and cell-to-cell virus transmission occurs very efficiently through intercellular synapses. The Journal of Infectious Diseases (JID) has devoted their December supplement to this important and understudied topic.
The 10 articles, four from researchers at BUSM, present the case for cell-associated HIV transmission as an important element contributing to the HIV epidemic. Anderson chides fellow researchers for not using cell-associated HIV in their transmission models: “The failure of several recent vaccine and microbicide clinical trials to prevent HIV transmission may be due in part to this oversight.”
Approximately 75 million people in the world have been infected with HIV-1 since the epidemic started over 30 years ago, mostly through sexual contact and maternal-to-child transmission. A series of vaccine and microbicide clinical trials to prevent HIV transmission have been unsuccessful, and scientists are returning to the drawing board to devise new approaches. The JID supplement advocates for new strategies that target HIV-infected cells in mucosal secretions.
The publication presents evidence that HIV-infected cells populate genital secretions from HIV-infected men and women as well as breast milk, and genetic evidence suggesting that cell-associated HIV transmission occurs in people. Various models for studying cell-associated HIV transmission and molecular targets for intervention are also presented. Finally, the efficacy of current HIV prevention strategies against cell-associated HIV transmission and opportunities for further development are described.
###
The collaborative team of BUSM researchers includes Drs. Deborah Anderson, Joseph Politch and Jai Marathe from the Departments of OB/GYN and Medicine, Manish Sagar from the Department of Medicine and Rahm Gummuluru from the Department of Microbiology. Collaborators include Drs. Roger LeGrand and Natalie DeJucq-Rainsford from France, Julie Overbaugh from the University of Washington, Tom Moench and Richard Cone from Johns Hopkins University, Kevin Whaley from Mapp Biopharmaceutical and Kenneth Mayer from Harvard Medical School. It is their hope that these articles will help to inform and invigorate the HIV prevention field and contribute to the development of more effective vaccine, treatment, and microbicide strategies for HIV prevention.
Funding was provided by the US National Institutes of Health (grant U19 AI096398) and the Fond de Dotation Pierre Berge, Sidation, France.
###
Gina DiGravio
[email protected]
617-638-8480
Boston University Medical Center
New technique provides novel approach to diagnosing ciliopathies
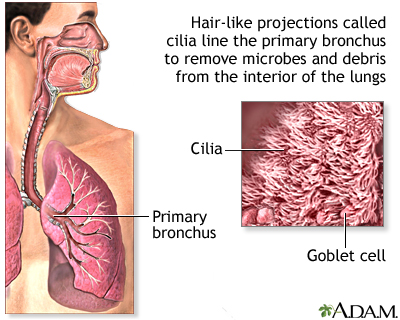
|
Cilia, the cell’s tails and antennas, are among the most important biological structures. They line our windpipe and sweep away all the junk we inhale; they help us see, smell and reproduce. When a mutation disrupts the function or structure of cilia, the effects on the human body are devastating and sometimes lethal.
The challenge in diagnosing, studying and treating these genetic disorders, called ciliopathies, is the small size of cilia—about 500-times thinner than a piece of paper. It’s been difficult to examine them in molecular detail until now.
Professor Daniela Nicastro and postdoctoral fellow Jianfeng Lin have captured the highest-resolution images of human cilia ever, using a new approach developed jointly with Lawrence Ostrowski and Michael Knowles from the University of North Carolina School of Medicine. They reported on the approach in a recent issue of Nature Communications.
About 20 different ciliopathies have been identified so far, including primary ciliary dyskinesia (PCD) and polycystic kidney disease (PKD), two of the most common ciliopathies. They are typically diagnosed through genetic screening and examination of a patient’s cilia under a conventional electron microscope.
The problem is, conventional electron microscopy is not powerful enough to detect all anomalies in the cilia, even when genetic mutations are present. As a result, the cause of ciliary malfunctions can be elusive and patients with ciliopathies can be misdiagnosed or undiagnosed.
Nicastro and her team developed an approach that includes advanced imaging technique that entails rapidly freezing human samples to preserve their native structure, imaging them with transmission electron microscopy, and turning those images into 3D models. This cutting-edge imaging was in part made possible by the advanced instrumentation in the Louise Mashal Gabbay Cellular Visualization Facility at Brandeis. It is the first time this approach has been used on human cilia and patient samples.
We have a new window into the structure and defects in human cilia.
“For so long, researchers haven’t been able to see the small defects in human cilia,” Nicastro says. “Now, we can fill in the pieces of the puzzle.”
###
Leah Burrows
[email protected]
781-736-4027
Brandeis University
UTSW researchers identify a therapeutic strategy that may treat a childhood neurological disorder

|
UT Southwestern Medical Center researchers have identified a possible therapy to treat neurofibromatosis type 1 or NF1, a childhood neurological disease characterized by learning deficits and autism that is caused by inherited mutations in the gene encoding a protein called neurofibromin.
Researchers initially determined that loss of neurofibromin in mice affects the development of the part of the brain called the cerebellum, which is responsible for balance, speech, memory, and learning.
The research team, led by Dr. Luis F. Parada, Chairman of Developmental Biology, next discovered that the anatomical defects in the cerebellum that arise in their mouse model of NF1 could be reversed by treating the animals with a molecule that counteracts the loss of neurofibromin.
“Children with neurofibromatosis have a high incidence of intellectual deficits and autism, syndromes that have been linked to the cerebellum and cortex,” said Dr. Parada, Director of the Kent Waldrep Foundation Center for Basic Neuroscience Research and holder of the Diana K. and Richard C. Strauss Distinguished Chair in Developmental Biology and the Southwestern Ball Distinguished Chair in Nerve Regeneration Research at UT Southwestern. “Our findings in these mouse models suggest that despite embryonic loss of the gene, therapies after birth may be able to reverse some aspects of the disease.”
The rare genetic disorder NF1, also known as von Recklinghausen disease, affects about 1 in 3,000 people and can lead to uncontrolled tumor growth along nerves. It also can result in behavioral, learning and autism spectrum disorders, trigger motor deficits, and impact aspects of memory and behavior.
Neurofibromin normally acts as a tumor suppressor, which keeps cells from growing and dividing too rapidly or in an uncontrolled way, according to the National Institutes of Health. Mutations in the NF1 gene lead to a nonfunctional version of neurofibromin that cannot regulate cell growth and division, which results in tumors such as neurofibromas that form along nerves throughout the body.
 The cerebellum, which consists of different layers formed by distinct cell types, continues to develop after birth. Before it can be fully formed, ‘immature’ nerve cells need to multiply and travel to the appropriate part of the cerebellum, where they ‘mature’ into the different nerve cell types to form the cerebellar layer. The UT Southwestern researchers saw that loss of neurofibromin interferes with this process, leading to a malformed cerebellum.
The cerebellum, which consists of different layers formed by distinct cell types, continues to develop after birth. Before it can be fully formed, ‘immature’ nerve cells need to multiply and travel to the appropriate part of the cerebellum, where they ‘mature’ into the different nerve cell types to form the cerebellar layer. The UT Southwestern researchers saw that loss of neurofibromin interferes with this process, leading to a malformed cerebellum.
In the absence of neurofibromin, the scientists found that a signaling pathway called ERK is always active, which interferes with normal brain development. With this information in hand, they treated newborn mice with inhibitors of the ERK pathway and found that the anatomical defects in the cerebellum could be reversed.
###
The findings are published in the journal Genes and Development. The work was supported by grants from the National Institutes of Health and the Simons Foundation.
Dr. Parada is an American Cancer Society Professor, and an elected member of the National Academy of Sciences; the American Academy of Arts and Sciences; the Institute of Medicine; and the American Association for the Advancement of Science.
Other UT Southwestern researchers involved in the work include postdoctoral researchers Dr. Efrain Sanchez-Ortiz, first author, and Dr. Inga Nazarenko, and former lab members Jian Chen, Woosung Cho, and Wei Mo.
About UT Southwestern Medical Center
UT Southwestern, one of the premier academic medical centers in the nation, integrates pioneering biomedical research with exceptional clinical care and education. The institution’s faculty includes many distinguished members, including six who have been awarded Nobel Prizes since 1985. Numbering approximately 2,800, the faculty is responsible for groundbreaking medical advances and is committed to translating science-driven research quickly to new clinical treatments. UT Southwestern physicians provide medical care in 40 specialties to about 92,000 hospitalized patients and oversee approximately 2.1 million outpatient visits a year.
###
Russell Rian
[email protected]
214-648-3404
UT Southwestern Medical Center
Advance Directives Can Benefit Patients, Families, and Health Care System

|
Nearly one out of four older Americans say that either they or a family member have experienced excessive or unwanted medical treatment, according to the latest issue of The Gerontological Society of America’s Public Policy & Aging Report (PP&AR), which goes on to show that Americans strongly support holding doctors accountable when they fail to honor patients’ end-of-life health care wishes.
This PP&AR, titled “Advanced Illness Care: Issues and Options,” features 12 articles that present new ways of understanding the complexity of securing appropriate advanced illness care and the decision-making dilemmas it presents. It also provides a valuable benefit by reviewing specific programs, demonstrations, and tools that family members and providers can use in providing care to persons with advanced illness. These models are person- and family-centered, and preliminary evaluations find that they may be cost-effective as well. Support for the publication was provided by Compassion & Choices.
“It is important to ensure that patients and their wishes are what drive the health care system, particularly at the end of life,” said Daniel R. Wilson, the national and federal programs director for Compassion & Choices. “We were pleased to partner with The Gerontological Society of America to publish this issue of the PP&AR, which includes cutting edge writers and thinkers in the advanced illness and end-of-life field.”
Advanced illness is defined as the period of illness when functioning and quality of life decline and where the efficacy of continued treatment is open to both medical and ethical question. Yet, as illness becomes more debilitating, clinical interventions often become more frequent. Studies show that the average Medicare beneficiary with one or more chronic conditions sees eight different physicians each year. It is at this stage when the medicalization of health care tends to overtake and overwhelm the needs and wishes of patients themselves. Advanced illness, due to disease, chronic conditions, or disability, can happen to anyone at any age. However, the vast majority of people with advanced illness are older than 65.
“Recent experience and studies make clear that well-informed individuals and their families often choose less care, in less institutional settings, often resulting in improved quality of life,” state Robert B. Hudson, PhD, and Brian W. Lindberg, MMHS, in their introduction to the issue. “It has become clear that palliative care and hospice care are often not provided soon enough, and that in-depth conversations with persons with advanced illness can help articulate treatment and life-style preferences that the health care system has often ignored or missed.”
Among the discussion of new models and tools that have been developed in recent years to better address advanced illness dilemmas and decisions, Charles Sabatino, JD, the director of the American Bar Association’s Commission on Law and Aging, highlights more than a dozen resources for updating and codifying preferences. He lists these under four headings: getting the conversation going, comprehensive advance planning tools, guides focusing on certain illnesses or decisions, and advance directive registries.
The new PP&AR comes on the heels of a major report released by the Institute of Medicine this fall, which was titled “Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life.” Its findings demonstrated that improving the quality and availability of medical and social services for patients and their families could not only enhance quality of life through the end of life, but may also contribute to a more sustainable care system.
###
Public Policy & Aging Report is a publication of the National Academy on an Aging Society, the policy branch of The Gerontological Society of America (GSA). As the nation’s oldest and largest interdisciplinary organization devoted to research, education, and practice in the field of aging, GSA’s principal mission - and that of its 5,500+ members - is to advance the study of aging and disseminate information among scientists, decision makers, and the general public. GSA’s structure also includes an educational branch, the Association for Gerontology in Higher Education.
###
Contact: Todd Kluss
[email protected]
(202) 587-2839
Step towards blood test for many cancer types
|
Scientists have identified more than 800 markers in the blood of cancer patients that could help lead to a single blood test for early detection of many types of cancer in future, according to research presented at the National Cancer Research Institute (NCRI) Cancer Conference in Liverpool today (Sunday).
This is the first time that cancer-specific blood markers have been comprehensively reviewed and identified for further clinical development. This study, by the UK Early Cancer Detection Consortium*, funded by Cancer Research UK, has analysed 19,000 scientific papers and found more than 800 biomarkers.
The aim of this research is to develop a screening test from a single blood sample for multiple cancer types. All cancers produce markers in the blood, so it could be feasible to develop a general screening test for many different forms of the disease.
In the UK, survival rates for cancer are lower than in some other western countries, part of which may be related to late diagnosis. But developing more ways to spot cancers earlier, including research into new screening technologies such as this, could help give more options for curative treatment, and save more lives in the future.
In the UK, cancer is most often detected after patients present symptoms to their doctor, with a small proportion being detected through any of the three national screening programmes for breast, bowel, and cervical cancer. This study could open the way for less invasive, new screening tests that could detect more cancers, possibly including some rare types, at an early stage when they are more likely to be treatable.
Cancer Research UK is committed to early diagnosis of cancer, importantly reducing late diagnosis and improving patients’ chances of surviving long term.
Study author Professor Ian Cree, a Cancer Research UK funded scientist at the University of Warwick and University Hospital in Coventry, said: “This is a new approach to early detection and the first time such a systematic review has been done. A single blood-based screening test would be a game changer for early detection of cancer which could help make it a curable disease for many more patients. We believe that we’ve identified all the relevant biomarkers; the next step is working out which ones work the best for spotting cancers.”
The identified biomarkers will be reviewed and categorised before they are developed further in clinical laboratory studies.
Sara Hiom, Cancer Research UK’s director of early diagnosis, said: “This is an innovative and promising new approach. And although in its early stages, it shows how our increased understanding of cancers’ ‘markers’ and new technologies are combining to offer new opportunities to detect cancer sooner. Diagnosing cancer at an early stage generally means more effective treatment and that translates into better survival. Our goal over the next 20 years is that three in four cancer patients will survive at least ten years after their diagnosis.”
###
For media enquiries please contact Stephanie McClellan on 020 3469 5314 or, out-of-hours, the duty press officer on 07050 264 059.
Notes to editors: *The Early Cancer Detection Consortium unites expertise from various disciplines including more than 20 universities, hospitals and commercial partners.
About the NCRI
The National Cancer Research Institute (NCRI) is a UK-wide partnership between the government, charity and industry. Its role is to promote cooperation in cancer research.
NCRI Partners are: the Association of the British Pharmaceutical Industry (ABPI); Biotechnology and Biological Sciences Research Council; Breakthrough Breast Cancer; Breast Cancer Campaign; Cancer Research UK; Children with Cancer UK; Department of Health; Economic and Social Research Council; Leukaemia & Lymphoma Research; Ludwig Institute for Cancer Research; Macmillan Cancer Support; Marie Curie Cancer Care; Medical Research Council; Northern Ireland Health and Social Care (Research & Development Office); Prostate Cancer UK; Roy Castle Lung Cancer Foundation; Scottish Government Health and Social Care Directorates (Chief Scientist Office); Tenovus; Welsh Government (National Institute for Social Care and Health Research); Worldwide Cancer Research (formerly the Association for International Cancer Research); Wellcome Trust; and Yorkshire Cancer Research.
About the NCRI Cancer Conference
The National Cancer Research Institute (NCRI) Cancer Conference is the UK’s major forum for showcasing the best British and international cancer research.
The Conference offers unique opportunities for networking and sharing knowledge by bringing together world-leading experts from all cancer research disciplines.
The tenth NCRI Cancer Conference is taking place from 2–5 November 2014 at the BT Convention Centre in Liverpool.
About the NIHR
The National Institute for Health Research (NIHR) is funded by the Department of Health to improve the health and wealth of the nation through research. Since its establishment in April 2006, the NIHR has transformed research in the NHS. It has increased the volume of applied health research for the benefit of patients and the public, driven faster translation of basic science discoveries into tangible benefits for patients and the economy, and developed and supported the people who conduct and contribute to applied health research. The NIHR plays a key role in the Government’s strategy for economic growth, attracting investment by the life-sciences industries through its world-class infrastructure for health research. Together, the NIHR people, programmes, centres of excellence and systems represent the most integrated health research system in the world.
###
Stephanie McClellan
[email protected]
44-020-346-95314
Cancer Research UK
Rare diseases: no reason for lower demands for studies

|
On behalf of the Federal Ministry of Health (BMG), the German Institute for Quality and Efficiency in Health Care (IQWiG) examined whether specific methodological aspects have to be considered in the conduct, analysis and assessment of the certainty of results of studies on rare diseases. Within the framework of the same commission, the Institute also analysed the underlying studies for the approval of so-called orphan drugs, i.e. drugs for rare diseases, in Europe.
The result: For a different approach than in more common diseases, there are neither scientific reasons nor specific designs and methods that would not also be relevant for more common diseases. This is the case for both drug and non-drug treatments. If compromises have to be made with regard to the reliability of the conclusions because of a particularly small number of participants, raising the significance level is preferable to a limitation of the external or even internal validity of the studies.
Focus on rare diseases
In the European Union diseases are classified as rare if they occur in not more than 5 per 10 000 inhabitants. Very rare diseases are diseases that affect fewer than 2 per 100 000 inhabitants. Of approximately 30 000 known diseases, 7000 to 8000 are considered rare, so that in Germany alone up to 4 million people are affected.
The German National Action League for People with Rare Diseases (NAMSE), founded in 2010, has developed a catalogue of policy proposals, which, among other things, includes the development of criteria for the assessment and analysis of studies with few participants. Against this background, the BMG awarded a two-part commission to IQWiG, which has now published the results in a so-called rapid report. Its contents follow the rapid report on the evidence in guidelines on rare diseases, which IQWiG produced in 2011, also on behalf of the BMG.
RCT as the gold standard
As explained in the IQWiG report, there are four key components that primarily determine the reliability of the conclusions of a study: the internal validity (i.e. the risk of bias), external validity (i.e. applicability), effect size, and precision of the results. The risk of bias can be minimized by randomization, double-blinding, and the so-called intention-to-treat principle, i.e. within the framework of randomized controlled trials (RCTs).
 Study sponsors occasionally argue that the methodological standards that are usually applied in clinical studies should be lowered for rare diseases. They justify this by claiming that RCTs are difficult to conduct due to the low number of participants, and that they are also ethically doubtful if effective comparator therapies are lacking. However, IQWiG reached a different conclusion: A low number of participants is equally problematic in all study types, and controlled studies are only ethically doubtful if the benefit or added benefit of the intervention under investigation is more or less proven already. However, further studies to clarify the question on benefit are then unnecessary anyway - not only in rare diseases.
Study sponsors occasionally argue that the methodological standards that are usually applied in clinical studies should be lowered for rare diseases. They justify this by claiming that RCTs are difficult to conduct due to the low number of participants, and that they are also ethically doubtful if effective comparator therapies are lacking. However, IQWiG reached a different conclusion: A low number of participants is equally problematic in all study types, and controlled studies are only ethically doubtful if the benefit or added benefit of the intervention under investigation is more or less proven already. However, further studies to clarify the question on benefit are then unnecessary anyway - not only in rare diseases.
Raising the significance level, if essential
Just like reduced internal validity, which increases the risk of bias, concessions on external validity can also lead to systematic errors, which cannot be adjusted for even with the most sophisticated statistical method.
Small effect sizes can only be determined with certainty by sufficiently large sample sizes in studies. Supraregional and international networks as well as disease registries that are as complete as possible are useful to collect a sufficient number of evaluable cases. The use of efficient statistical methods, e.g. sequential study designs, may allow for smaller sample sizes without affecting internal or external validity.
If this is not sufficient in the case of very rare diseases, IQWiG recommends compromising on precision: raising the significance level, e.g. from the usual five to ten percent, to obtain statistically significant results despite a small sample size. This makes it possible to at least quantify the probability of error: The uncertainty of a decision is known.
Empirical data support methodological expertise
For the second goal of the commission, IQWiG examined all 85 drug approvals for rare and very rare diseases in Europe between 2001 and 2013. 82 out of the 125 studies submitted within the framework of these approvals were RCTs, which clearly shows that it is not necessary to compromise on methodology. Most studies were multicentre, multinational, and multicontinental. Specific statistical methods aiming for high efficiency were used in about two thirds of the studies.
All patients have a right to quality
“It has been shown that in studies on rare diseases, deviation from the methods usually applied in studies is neither necessary nor possible without compromising on quality”, concludes the Institute’s Director Jürgen Windeler. “In most cases, reservations concerning RCTs in rare diseases are unwarranted.”
The EU regulation No. 141/2000 already stipulated that patients suffering from rare conditions should be entitled to the same drug quality, safety and efficacy as other patients and that orphan drugs should therefore be subjected to the normal evaluation process. “The best way to do justice to these requirements is to conduct multicentre RCTs, in which the risk of bias is minimized and the data recorded are carefully analysed”, says Windeler. “This makes it possible to estimate with sufficient certainty the benefit and harm of the intervention for the people affected, despite the small numbers of participants.”
Process of report production
The BMG commissioned IQWiG in December 2013. The report was to be prepared in an accelerated procedure as a “rapid report”. In contrast to the usual procedure, no preliminary reports are published here. Although a draft version of the report is reviewed by external experts, no hearing at which all interested parties can comment takes place. The report was sent to the commissioning agency on 8 September 2014.
An overview of the background, methods and further results of the report is provided in the following executive summary.
###
Phone+49 (0)221 - 35685-0
[email protected]
Responsibilities and objectives of IQWiG
Findings point to an ‘off switch’ for drug resistance in cancer

|
Like a colony of bacteria or species of animals, cancer cells within a tumor must evolve to survive. A dose of chemotherapy may kill hundreds of thousands of cancer cells, for example, but a single cell with a unique mutation can survive and quickly generate a new batch of drug-resistant cells, making cancer hard to combat.
Now, scientists at the Salk Institute have uncovered details about how cancer is able to become drug resistant over time, a phenomenon that occurs because cancer cells within the same tumor aren’t identical- the cells have slight genetic variation, or diversity. The new work, published October 20 in PNAS, shows how variations in breast cancer cells’ RNA, the molecule that decodes genes and produces proteins, helps the cancer to evolve more quickly than previously thought. These new findings may potentially point to a “switch” to turn off this diversity- and thereby drug resistance- in cancer cells.
“It’s an inherent property of nature that in a community- whether it is people, bacteria or cells- a small number of members will likely survive different types of unanticipated environmental stress by maintaining diversity among its members,” says the senior author of the new work, Beverly Emerson, professor of Salk’s Regulatory Biology Laboratory and holder of the Edwin K. Hunter Chair. “Cancer co-ops this diversification strategy to foster drug resistance.”
Instead of looking at a single gene or pathway to target with cancer therapies, lead author Fernando Lopez-Diaz, Salk staff scientist, and the team aim to uncover the diversification “switch” by which cancer cells replicate but vary slightly from one another. Turning off this cellular process would strip cancer’s ability to survive drug treatment.
“Cancer isn’t one cell but it’s an ecosystem, a community of cells,” says Emerson. “This study begins the groundwork for potentially finding a way to understand and dial back cell diversity and adaptability during chemotherapy to decrease drug resistance.”
To uncover how groups of cancer cells achieve functional diversity (through RNA) to survive chemotherapy, Lopez-Diaz dosed dishes of human pre-cancer and metastatic breast cancer cells with the cancer drug paclitaxel for a week and then removed the drug for a few weeks, mimicking the treatment cycle for a cancer patient. Surviving cells- usually one or two out of millions- began to repopulate but with subtle changes in their RNA, presumably enabling them to survive future doses of the cancer drug.
By pushing the boundaries of bioinformatics, a collaboration led by Mei-Chong Wendy Lee and Nader Pourmand at the University of California, Santa Cruz charted more than 80,000 pieces of RNA per new cancer cell- typically, single-cell studies by other approaches look at hundreds or so RNA pieces to distinguish fairly different cells from one another. This unusually thorough list helped the researchers tease out subtle differences between generations of same cancer cells treated with chemotherapy and chart how the cancer cell community increased diversity among its members through RNA.
“We found an overwhelming return to diversity after chemotherapy treatment that couldn’t be explained by expected mechanisms,” says Lopez-Diaz. “There is something else going on here, a ‘philosopher’s stone’ to cancer cell diversity that we now know to look for.”
IMAGE: This image shows, from the left: Yelena Dayn, Fernando Lopez-Diaz, Beverly Emerson.
Click here for more information.
And when the team analyzed the gene expression profiles of the surviving cancer cell line, they were again surprised. “We thought they’d look like stressed cells with a few changes,” says Emerson. “Instead, after a few population doublings they go back to the normal gene expression pattern and rapidly reacquired drug sensitivity.” This adaptive behavior, Emerson speculates, lets the group of cancer cells prepare for the next unanticipated threat.
Another intriguing finding of the paper was that a high percentage of precancerous cells that underwent chemotherapy survived and proliferated, more so than either normal or cancerous cells. This led the pre-cancer cells to become more drug tolerant once they became a tumor. “The pre-cancer cells, when exposed to chemotherapy, evolved much faster and create a more drug-resistant state,” says Lopez-Diaz. “This and other findings can now be explored into greater detail using the knowledge and perspective we have gained here.”
###
Authors of the work include Beverly M. Emerson, Fernando J. Lopez-Diaz and Yelena Dayn at the Salk Institute; Nader Pourmand, Mei-Chong Wendy Lee, Shahid Yar Khan, Muhammad Akram Tariq, Amie J. Radenbaugh, and Hyunsung John Kim of the University of California, Santa Cruz; and Charles Joseph Vaske of Five3 Genomics.
Funding for the work includes support from the National Institutes of Health, the Chambers Medical Foundation, the GemCon Family Foundation and the Olive Tupper Foundation.
About the Salk Institute for Biological Studies ?
The Salk Institute for Biological Studies is one of the world’s preeminent basic research institutions, where internationally renowned faculty probes fundamental life science questions in a unique, collaborative, and creative environment. Focused both on discovery and on mentoring future generations of researchers, Salk scientists make groundbreaking contributions to our understanding of cancer, aging, Alzheimer’s, diabetes and infectious diseases by studying neuroscience, genetics, cell and plant biology, and related disciplines.
Faculty achievements have been recognized with numerous honors, including Nobel Prizes and memberships in the National Academy of Sciences. Founded in 1960 by polio vaccine pioneer Jonas Salk, MD, the Institute is an independent nonprofit organization and architectural landmark.
#$##
Salk Communications
[email protected]
Salk Institute
Siblings of children with autism can show signs at 18 months

|
About 20% of younger siblings of children with Autism Spectrum Disorder (ASD) will develop the condition by age 3. A new study by Yale School of Medicine researchers has found that 57% of these younger siblings who later develop the condition already showed symptoms at age 18 months.
Published in the October Journal of the American Academy of Child & Adolescent Psychiatry, this is the first large-scale, multi-site study aimed at identifying specific social-communicative behaviors that distinguish infants with ASD from their typically and atypically developing high-risk peers as early as 18 months of age.
“While the majority of siblings of children with ASD will not develop the condition themselves, for those who do, one of the key priorities is finding more effective ways of identifying and treating them as early as possible,” said lead author Katarzyna Chawarska, associate professor in the Yale Child Study Center and the Department of Pediatrics at Yale School of Medicine. “Our study reinforces the need for repeated diagnostic screening in the first three years of life to identify individual cases of ASD as soon as behavioral symptoms are apparent.”
Chawarska and her co-authors pooled data from eight sites participating in the Autism Speaks Baby Siblings Research Consortium. The team closely examined social, communicative, and repetitive behaviors in 719 infants when they were 18 months old. The team looked for patterns that might predict a later diagnosis of ASD. They then followed up when the participants were age 3.
“Our research suggests that approximately half of the siblings who are later diagnosed with ASD display signs suggestive of ASD at 18 months, and in those who appeared asymptomatic at 18 months, symptoms appeared between 18 and 36 months,” said Chawarska.
Chawarska said what was most interesting to the research team was that different patterns of behaviors at 18 months may be predictive of ASD later on. In about 50% of siblings, a combination of poor eye contact and lack of communicative gestures or imaginative play is most strongly associated with later ASD diagnosis. In a small percentage of those later diagnosed with ASD, eye contact may be relatively normal, but they begin to display early signs of repetitive behaviors and have limited non-verbal communication skills.
“So not only do the behavioral symptoms appear at different ages, but different combinations of early symptoms may predict the diagnostic outcome,” Chawarska added. “Linking these developmental dynamics with underlying neurobiology may advance our understanding of causes of ASD and further efforts to personalize treatment for ASD by tailoring it to specific clinical profiles and their developmental dynamics.”
###
Other authors on the study included Suzanne Macari, Frederick Shic, Daniel J. Campbell, Jessica Brian, Rebecca Landa, Ted Hutman, Charles A. Nelson, Sally Ozonoff, Helen Tager-Flusberg, Gregory S. Young, Lonnie Zwaigenbaum, Ira L. Cohen, Tony Charman, Daniel S. Messinger, Ami Klin, Scott Johnson, and Susan Bryson.
Citation: JACC doi: 10.1016/j.jaac.2014.09.015
###
Karen N. Peart
[email protected]
203-432-1326
Yale University
University of Calgary research leads to brain cancer clinical trial

|
Researchers at the University of Calgary’s Hotchkiss Brain Institute (HBI) and Southern Alberta Cancer Research Institute (SACRI) have made a discovery that could prolong the life of people living with glioblastoma - the most aggressive type of brain cancer. Samuel Weiss, PhD, Professor and Director of the HBI, and Research Assistant Professor Artee Luchman, PhD, and colleagues, published their work today in Clinical Cancer Research, which is leading researchers to start a human phase I/II clinical trial as early as Spring 2015.
Researchers used tumour cells derived from 100 different glioblastoma patients to test drugs that could target the disease. When these human brain tumour-initiating cells were inserted into an animal model, researchers discovered that when using a drug, AZD8055, combined with Temozolomide (TMZ) - a drug already taken by most glioblastoma patients - the life of the animals was extended by 30 per cent.
“Shutting off vital tumour growth processes can lead to the death of human brain tumour-initiating cells. Our research has identified a key process in brain tumour growth that we were able to target with AZD8055,” says Luchman from the university’s Cumming School of Medicine and a member of the HBI.
Researchers used the new therapy to inhibit a pathway in the cancer cells known as mTOR signaling - putting the brakes on this pathway, combined with the current standard therapy, caused more of the cancer cells to die. Scientists are now working with investigators at the NCIC Clinical Trials Group (NCIC-CTG) to start a Canadian clinical trial that may eventually include glioblastoma patients across the country.
“Discovering new pathways and therapies that can be tested in the clinic provides the greatest hope for brain cancer patients and their families,” says Weiss, leader of the university’s Brain and Mental Health strategic research priority.
Glioblastoma is the most common and deadly form of brain cancer among adults. The progression and complexity of the tumours are often difficult to treat. The median survival for patients is 15 months, with less than five per cent of patients surviving beyond five years.
University of Calgary researchers including Luchman, Weiss and Dr. Greg Cairncross – director of SACRI, and leader of the Terry Fox Research Institute (TFRI) ‘Therapeutic Targeting of Glioblastoma research program at the university - are now working with cancer researchers Dr. Warren Mason (Princess Margaret Cancer Centre in Toronto) and Dr. Lesley Seymour (Director of the NCIC Clinical Trials Group’s Investigational New Drug Program), and drug manufacturer AstraZeneca, to plan a clinical trial testing a similar, but newer, drug related to AZD8055 (called AZD2014), in combination with TMZ, in patients with glioblastoma.
“This is an important initiative - to test new drugs, being developed for other types of cancers in the laboratory to identify which are most promising for testing in patients with glioblastoma. NCIC CTG is excited to partner in the development of this clinical trial, which will be funded by a grant from the TFRI as well as grants from Canadian Cancer Society Research Institute to NCIC CTG,” says Seymour.
###
The study was funded by the Alberta Cancer Foundation, Alberta Innovates-Health Solutions and the Canadian Stem Cell Network.
###
Marta Cyperling
[email protected]
403-210-3835
University of Calgary, Faculty of Medicine
Exploring the connection between empathy, neurohormones and aggression
|
Empathy is typically seen as eliciting warmth and compassion -a generally positive state that makes people do good things to others. However, empathy may also motivate aggression on behalf of the vulnerable other. Researchers at the State University of New York at Buffalo, examined whether assessed or elicited empathy would lead to situation-specific aggression on behalf of another person, and to explore the potential role of two neurohormones in explaining a connection between empathy and aggression. The study is published in Personality and Social Psychology Bulletin.
Design of the Study
Empathic impulses are aimed at reducing the suffering of the target of empathy. Sometimes aggression may be the response that is perceived to best address the need of the other, or best suited to end their suffering. This effect may, in part, be due in part to physiological changes that occur in the body as a result of empathy. The research focused on two neurohormones, oxytocin and vasopressin. Oxytocin has been associated with empathy in previous research, and also with protective aggression. Vasopressin has been much more commonly studied in the animal literature, but has similarly been associated with aggression to defend a mate or offspring.
The first study asked participants to write and answer questions about a time in the past 12 months where they witnessed a close other being hurt physically or emotionally by a third party other than themselves. The results illustrate that empathy, not trait aggression or perceptions of emotional threat toward the self, motivated predicted aggression of the participants.
The second study involved an empathy manipulation and a distress manipulation. Participants were given a scenario describing someone having financial difficulty, and that person was either worried (high need) or not (low need). Half the participants were told to read the scenario with instructions that were empathy-inducing, and half were not. Participants were also told this person would engage in a competitive task with another individual, and participants were given the opportunity to sabotage the performance of the other individual by assigning that person a certain amount of hot sauce to drink. “Hot sauce was described to them as a clearly painful and performance hindering substance, meaning that the more hot sauce they assigned, the worse the anonymous person would do on the task…and presumably, the more likely that the person with financial troubles could win,” explains lead researcher Anneke Buffone.
Results of the Study
Participants who felt empathy in the Study 1 were more likely to aggress against the close other’s perpetrator if the close other was perceived to be distressed, but not when the close other was not perceived to be distressed. The empathy manipulation in the Study 2 increased aggression (the amount of hot sauce assigned) toward the target’s competitor, but only when the empathy target was described as distressed. The results of study 2 demonstrate that empathy-linked aggression can occur for a stranger, and that provocation by the target is unlikely to be the sole mechanism for empathy-linked aggression.
The participants contributed saliva samples for analysis of their neurohormone gene variants. In both studies, participants with a short/short version of the 1a vasopressin receptor (AVPR1a) showed less aggression, while those with a long version of the receptor showed higher aggression. The pattern is consistent with the possibility that vasopressin facilitates empathic responses, including aggression, to individuals in need. In one study, individuals with one oxytocin receptor genotype, OXTR rs53576 GG showed greater aggression than those with the AA/AG genotype.
The study ruled out certain variables, such as trait aggression and impulsiveness. “Aggression is known to result from characteristics such as impulsiveness, trait aggression, trait or state anger. We wanted to rule out these motivators of aggression because our argument is that anyone can act aggressively out of an empathic impulse, not just those with a certain personality,” Buffone elaborates. “We think that among situational motivators of aggression, witnessing the suffering or need of others people have come to care about has been largely overlooked.”
The findings of the research provide evidence that activating empathy may prompt aggression toward those in conflict or competition with empathy targets, even independent of traditional predictors of aggression and in the absence of wrongdoing or provocation from the target of aggression. Empathy could even lead an individual to blame an innocent person for a crime or misdeed to protect a friend or child from punishment. And it is even possible that feeling empathy for strangers perceived to be treated unjustly might motivate aggression on their behalf. In all of these cases, empathy can lead more directly to aggression- anger isn’t always necessary.
###
Please email [email protected] if you would like a copy of the original study in Personality and Social Psychology Bulletin.
Buffone, A.E., Poulin, M.J. (2014). Empathy, Target Distress, and Neurohormone Genes Interact to Predict Aggression for Others - Even Without Provocation. Personality and Social Psychology Bulletin, 40(11).
Personality and Social Psychology Bulletin (PSPB), published monthly, is an official journal of the Society of Personality and Social Psychology (SPSP). SPSP promotes scientific research that explores how people think, behave, feel, and interact. The Society is the largest organization of social and personality psychologists in the world. Follow us on Twitter, @SPSPnews and find us at facebook.com/SPSP.org
###
Jennifer Santisi
[email protected]
202-524-6543
Society for Personality and Social Psychology
U.S. nutrition program for mothers, infants sees falling demand

|
A government nutrition program for pregnant mothers and small children has not kept pace with technology and U.S. poverty experts say its paper voucher system is driving low-income women away from the program when they need it most.
The Special Supplemental Nutrition Program for Women, Infants and Children, known as WIC, has seen a sharp drop in participation since 2010, unlike food stamps and other anti-poverty programs that ballooned during the 2007-9 recession and the economic recovery that followed, government figures show.
“WIC providers are tearing their hair, beating their chests, ‘what are they doing wrong?’” said Laurie True, California WIC Association director.
Poverty experts say the shrinking demand does not reflect less need. They are pushing for faster changes to an outdated, cumbersome distribution process they say stigmatizes recipients.
Participants complain of customers “shaming” them in grocery lines, said Sarah Monje, California’s Native American Health Center WIC director.
“I can feel the aura: ‘Oh my god, this girl is taking forever,’” said WIC recipient Marquel Davis of Austin, Texas.
With a generation of Americans “used to getting everything on their smartphones,” True said, WIC is still “stuck in the hands-on experience.”
“That doesn’t make the program as attractive to people who may be on the border lines, the working poor and very busy - most of our participants work at least one job,” she said.
Congress mandated in 2010 that WIC switch to electronic benefit cards by 2020. All but nine U.S. states still rely on paper vouchers that program directors say hold up grocery-store lines and embarrass mothers.
 Davis, 26, said it was a hassle trying to redeem her WIC checks before Texas switched to an electronic system several years ago. The program pays only for specified foods sold in certain quantities.
Davis, 26, said it was a hassle trying to redeem her WIC checks before Texas switched to an electronic system several years ago. The program pays only for specified foods sold in certain quantities.
“You’ve got to separate [your groceries] and make sure it’s the right one, right size, and on top of that, you got to sign and they got to initial,” Davis said. “It’s just hectic, especially if you have a kid shopping with you and you’re trying to get home.”
WIC gives low-income pregnant, post-partum or breastfeeding women and kids up to age five vouchers worth about $43 each month for formula and healthy foods that adhere to federal nutrition requirements, such as limiting added sugar in yogurt and mandating that bread include whole wheat flour.
The program requires recipients to attend classes on eating well and breastfeeding.
Though WIC grew fairly steadily since its inception in 1972, U.S. Department of Agriculture data shows it shrank 10.6 percent between fiscal year 2010 and May 2014.
Staff members “don’t have a sense of declining need in their communities,” said analyst Zoe Neuberger of the Center on Budget and Policy Priorities, a poverty-focused think tank.
Participants dropped from 9.2 million to 8.2 million from 2010 to May, decreasing in every state and the District of Columbia, according to USDA. In Georgia, caseload plummeted 46 percent since 2009.
Conversely, food stamp enrollment skyrocketed from 28.2 million in 2008 to 47.6 million in 2013 under expansions in President Barack Obama’s 2009 stimulus package, though it fell to 46.2 million in May after benefits expired last November.
But the smaller, more targeted WIC started shrinking years earlier and to a greater extent relative to enrollment, USDA data shows.
SOCIAL STIGMA
The social stigma, always a factor for some people, was accentuated by a distribution system largely unchanged in four decades, directors said.
Many women have switched to food stamps, which use a debit-like card but lack such WIC benefits as affording expensive baby formula, feeding children healthier food and learning workplace breastfeeding rights, directors said.
Being required to attend WIC advising sessions every one to three months can be a problem for low-income workers.
Those include illegal immigrants, who may be deterred over fear of an immigration crackdown, New York-based nonprofit Community Food Advocates co-founder Agnes Molnar said. The WIC program does not require proof of citizenship, though state or tribal residency is required.
Michael Osur, who runs 18 WIC clinics in southern California’s Riverside County, saw an almost 40 percent drop in the percentage of people requesting materials in Spanish from 2007 to 2013.
Lingering effects from last October’s government shutdown, when clinics shuttered or scraped by on reserve funds, also hurt WIC, National WIC Association CEO Douglas Greenaway said.
If caseload continues to drop, Congress will cut funding and clinics will close, consolidate and limit overtime and weekend services, True said.
In California, Osur was opening mobile neighborhood clinics, insisting many women were neglecting critical help.
“I think the need is there,” he said. “We’ve just got to find a way to reach them.”
###
(Reuters)
A better way to track emerging cell therapies using MRIs

|
Cellular therapeutics – using intact cells to treat and cure disease – is a hugely promising new approach in medicine but it is hindered by the inability of doctors and scientists to effectively track the movements, destination and persistence of these cells in patients without resorting to invasive procedures, like tissue sampling.
In a paper published September 17 in the online journal Magnetic Resonance in Medicine, researchers at the University of California, San Diego School of Medicine, University of Pittsburgh and elsewhere describe the first human tests of using a perfluorocarbon (PFC) tracer in combination with non-invasive magnetic resonance imaging (MRI) to track therapeutic immune cells injected into patients with colorectal cancer.
“Initially, we see this technique used for clinical trials that involve tests of new cell therapies,” said first author Eric T. Ahrens, PhD, professor in the Department of Radiology at UC San Diego. “Clinical development of cell therapies can be accelerated by providing feedback regarding cell motility, optimal delivery routes, individual therapeutic doses and engraftment success.”
Currently, there is no accepted way to image cells in the human body that covers a broad range of cell types and diseases. Earlier techniques have used metal ion-based vascular MRI contrast agents and radioisotopes. The former have proven difficult to differentiate in vivo; the latter raise concerns about radiation toxicity and do not provide the anatomical detail available with MRIs.
“This is the first human PFC cell tracking agent, which is a new way to do MRI cell tracking,” said Ahrens. “It’s the first example of a clinical MRI agent designed specifically for cell tracking.”
Researchers used a PFC tracer agent and an MRI technique that directly detects fluorine atoms in labeled cells. Fluorine atoms naturally occur in extremely low concentrations in the body, making it easier to observe cells labeled with fluorine using MRI. In this case, the modified and labeled dendritic cells – potent stimulators of the immune system – were first prepared from white blood cells extracted from the patient. The cells were then injected into patients with stage 4 metastatic colorectal cancer to stimulate an anti-cancer T-cell immune response.
The published study did not assess the efficacy of the cell therapy, but rather the ability of researchers to detect the labeled cells and monitor what happened to them. Ahrens said the technique worked as expected, with the surprising finding that only half of the delivered cell vaccine remained at the inoculation site after 24 hours.
“The imaging agent technology has been to shown to be able to tag any cell type that is of interest,” Ahrens said. “It is a platform imaging technology for a wide range of diseases and applications,” which might also speed development of relevant therapies.
“Non-invasive cell tracking may help lower regulatory barriers,” Ahrens explained. “For example, new stem cell therapies can be slow to obtain regulatory approvals in part because it is difficult, if not impossible, with current approaches to verify survival and location of transplanted cells. And cell therapy trials generally have a high cost per patient. Tools that allow the investigator to gain a ‘richer’ data set from individual patients mean it may be possible to reduce patient numbers enrolled in a trial, thus reducing total trial cost.”
###
Co-authors include Brooke M. Helfer and Charles F. O’Hanlon, Celsense, Inc. Pittsburgh; and Claudiu Schirda, University of Pittsburgh.
Funding support came, in part, from the National Institutes of Health (grant R01-CA13463) and the California Institute for Regenerative Medicine.
###
Scott LaFee
[email protected]
619-543-6163
University of California - San Diego
New superfoods could help key protein keep bodies healthy
|
|
A new generation of new superfoods that tackle heart disease and diabetes could be developed following research into a protein that helps keep cells in our bodies healthy.
Researchers at the University of Warwick found that the protein, called Nrf2, continually moves in and out of the nuclei of human cells to sense the cell’s health and vitality.
When Nrf2 is exposed to threats to the cell’s health it oscillates faster and activates an increase in the cell’s defence mechanism, including raising the levels of antioxidant.
The researchers, from the University’s Warwick Medical School, successfully increased the speed of Nrf2’s movement by artificially introducing health beneficial substances – potential components of new superfoods.
The beneficial substances comprise broccoli-derived sulforaphane and quercetin, which is found in high-levels in onions.
The team used these insights to develop new food supplements, which are currently being trialled to decrease risk of developing diabetes and heart disease.
Published by Antioxidants and Redox Signalling, the research investigated the ways in which compounds in fruit and vegetables keep humans healthy.
Oxidative stress in health and disease: The therapeutic potential of Nrf2 activation
For the past 40 years or so, oxidative stress has been increasingly recognized as a contributing factor in aging and in various forms of pathophysiology generally associated with aging. Our view of oxidative stress has been largely “superoxide-centric”, as we focused on the pathological sources of this oxygen-derived free radical and the types of molecular havoc it can wreak, as well as on the protection provided by the antioxidant enzymes, especially the superoxide dismutases, catalases, and glutathione peroxidases. In the last decade our view of oxidative stress has broadened considerably, and it is now often seen as an imbalance that has its origins in our genes, and the ways in which gene expression is regulated. At the center of this new focus is the transcription factor called nuclear factor (erythroid-derived 2)-like 2, or Nrf2. Nrf2 is referred to as the “master regulator” of the antioxidant response, modulating the expression of hundreds of genes, including not only the familiar antioxidant enzymes, but large numbers of genes that control seemingly disparate processes such as immune and inflammatory responses, tissue remodeling and fibrosis, carcinogenesis and metastasis, and even cognitive dysfunction and addictive behavior. Thus, the dysregulation of Nrf2-regulated genes provides a logical explanation for the connections, both direct and indirect, between observable oxidative stress and perhaps 200 human diseases involving these various physiological processes, each reflecting a network involving many gene products. The evolutionary self-association of these many genes under the common control of Nrf2 suggests that the immune and inflammatory systems may present the largest demand for increased antioxidant protection, apart from constitutive oxidative stress resulting from mitochondrial oxygen consumption for metabolic purposes. Gene expression microarray data on human primary vascular endothelial cells and on the SK-N-MC human neuroblastoma-derived cell line have been obtained in response to the dietary supplement Protandim, a potent composition of highly synergistic phytochemical Nrf2 activators. Pathway analysis of results shows significant modulation by Protandim of pathways involving not only antioxidant enzymes, but of those related to colon cancer, cardiovascular disease, and Alzheimer disease.
###
Brooks M. Hybertson ,
Bifeng Gao, ,
Swapan K. Bose ,
Joe M. McCorda
The research team are the first to record the continual movement cycle of Nrf2, which sees the protein oscillate in and out of the cell nucleus once every 129 minutes. When stimulated by a health beneficial vegetable-derived substance Nrf2’s cycle sped up to 80 minutes.
Lead researcher Professor Paul Thornalley says, “The way Nrf2 works is very similar to sensors in electronic devices that rely on continual reassessment of their surroundings to provide an appropriate response”.
Discussing the health benefits of the research Professor Thornalley argues:
“The health benefit of Nrf2 oscillating at a fast speed is that surveillance of cell health is increased when most needed, that is, when cells are under threat. By understanding how this process works and increasing Nrf2’s speed without putting cells under threat, new strategies for design of healthier foods and improved drugs can be devised. Current designs may have selected substances with suboptimal if not poor health benefits in some cases.”
Nrf2, a guardian of healthspan and gatekeeper of species longevity
Although aging is a ubiquitous process that prevails in all organisms, the mechanisms governing both the rate of decline in functionality and the age of onset remain elusive. A profound constitutively upregulated cytoprotective response is commonly observed in naturally long-lived species and experimental models of extensions to lifespan (e.g., genetically-altered and/or experimentally manipulated organisms), as indicated by enhanced resistance to stress and upregulated downstream components of the cytoprotective nuclear factor erythroid 2-related factor 2 (Nrf2)-signaling pathway. The transcription factor Nrf2 is constitutively expressed in all tissues, although levels may vary among organs, with the key detoxification organs (kidney and liver) exhibiting highest levels. Nrf2 may be further induced by cellular stressors including endogenous reactive-oxygen species or exogenous electrophiles. The Nrf2-signaling pathway mediates multiple avenues of cytoprotection by activating the transcription of more than 200 genes that are crucial in the metabolism of drugs and toxins, protection against oxidative stress and inflammation, as well as playing an integral role in stability of proteins and in the removal of damaged proteins via proteasomal degradation or autophagy. Nrf2 interacts with other important cell regulators such as tumor suppressor protein 53 (p53) and nuclear factor-kappa beta (NF-κB) and through their combined interactions is the guardian of healthspan, protecting against many age-related diseases including cancer and neurodegeneration. We hypothesize that this signaling pathway plays a critical role in the determination of species longevity and that this pathway may indeed be the master regulator of the aging process.
Commenting on the research, Professor Andreu Palou, coordinator of the EU-funded BIOCLAIMS research programme said “A main nutritional challenge in Europe is to substantiate the beneficial effects of foods that are advertised to the consumers. The approach of the group of Prof Thornalley is opening a fascinating new window.”
###
11 September 2014
Notes for Editors:
For a copy of the paper or to speak with Professor Thornalley please email Tom Frew; [email protected]
The research was funded by the Biotechnology and Biosciences Research Council UK (BBSRC) Diet and Health Research Industry Club (DRINC) and the EU Framework Programme-7 BIOmarkers of Robustness of Metabolic Homeostasis for Nutrigenomics-derived Health CLAIMS Made on Food (BIOCLAIMS) project.
The research was performed by collaboration between the Medical School, Life Sciences and Systems Biology Centre at the University of Warwick: Drs Mingzhan Xue, Hiroshi Momiji, Naila Rabbani, Guy Barker, Till Bretschneider and Tony Shmygol, and Profs David Rand and Paul Thornalley.
###
Tom Frew
[email protected]
44-024-767-75910
University of Warwick
@warwickuni
Mobile app on emergency cardiac care aids best decisions in seconds

|
Saturday 30 August 2014: The ACCA Clinical Decision-Making Toolkit mobile app is now available on the App Store and Google Play.
When dealing with acute cardiovascular diseases, a few seconds can make the difference and instant access to the best recommendations can save lives. This led the Acute Cardiovascular Care Association (ACCA) of the ESC to develop a user friendly interactive application, allowing professionals to have immediate access to diagnostics pathways on their mobile devices.
The Toolkit on emergency cardiac care, first published as a pocket-sized manual, is helping practitioners across the globe to make the best decisions in seconds. The Toolkit was created by expert members of ACCA and can be downloaded here.
Professor Héctor Bueno, President Elect and Acting President of ACCA and Editor in Chief of the Toolkit, said: “We have created the first tool to help all healthcare professionals who treat patients with acute cardiovascular syndromes to make the correct decisions fast.”
Dr Pascal Vranckx, Associate Editor of the Toolkit, said: “The Toolkit has been enormously successful. To date, 12 500 clinicians have received the pocket version and 15 000 copies have been downloaded from the ESC website. Clinicians tell us that it is now the tool to use in daily practice.”
The Toolkit is based on ESC Clinical Practice Guidelines(1-5) and was written by European experts and opinion leaders in acute cardiovascular care. The seven chapters cover symptoms (chest pain, dyspnea, syncope), acute coronary syndromes, acute heart failure, cardiac arrest and cardiopulmonary resuscitation (CPR), rhythm disturbances, acute vascular syndromes, and acute myocardial/pericardial syndromes.
 During ACCA’s annual summit on pre-hospital care in April, delegates cited the numerous benefits of using the Toolkit in their daily practice treating emergency cardiac patients. Dr Vaya Agladze from Tbilisi, Georgia, said: “The ACCA Toolkit will help us save lives, which is the main goal of doctors in every country. The charts and tables clearly show the treatment a patient needs and are a quick guide for paramedics in ambulances, doctors and nurses in emergency rooms, and cardiologists.”
During ACCA’s annual summit on pre-hospital care in April, delegates cited the numerous benefits of using the Toolkit in their daily practice treating emergency cardiac patients. Dr Vaya Agladze from Tbilisi, Georgia, said: “The ACCA Toolkit will help us save lives, which is the main goal of doctors in every country. The charts and tables clearly show the treatment a patient needs and are a quick guide for paramedics in ambulances, doctors and nurses in emergency rooms, and cardiologists.”
Dr Zaza Iakobishvili from Petah Tikva, Israel, said: “Half of our patients are transferred by ambulance with paramedics who may be unsure if they are facing a real cardiac emergency or not. The Toolkit is a tremendous resource in these cases, shortening delays in making a correct diagnosis and ensuring that patients get appropriate treatment fast.”
Dr Sofie Gevaert from Gent, Belgium, said: “All of the essential messages are in the Toolkit, which deals with the whole spectrum of acute cardiac care, from patient symptoms to providing the right diagnosis and treatment. This makes it great for teaching young doctors. We also use it to brief non-cardiac physicians in emergency and intensive care on how to provide the best standard of care for acute cardiac patients.”
Professor Helmy Elghawaby from Cairo, Egypt, said: “By using the Toolkit we are ensuring that our whole emergency cardiac care team, which includes paramedics in the ambulance, doctors and nurses in the emergency room, and cardiologists, are providing the same high quality care. Everyone in the team carries one in their pocket and it takes just seconds to consult the tables and treatment algorithms.”
Professor Bueno said: “The mobile app can be used on smartphones and tablets. We plan to translate the Toolkit into other languages, including Spanish, Portuguese and Russian, making it accessible to an even greater number of professionals involved in acute cardiovascular care. A second edition is on the way with additional chapters addressing other relevant questions that occur in acute cardiovascular care settings.”
Dr Vranckx said: “We will update the Toolkit each year as the guidelines incorporate new scientific evidence. This process will be made easier with the app. In this way we will ensure that the Toolkit always provides the most appropriate information to help clinicians in their daily practice.”
Professor Bueno concluded: “Our main goal is to help standardise quality of care for acute cardiac patients in Europe in the prehospital phase and across hospital departments. Clinicians say the Toolkit assists them in the field and the additions, updates and app should make it even more useful.”
###
References
(1) Guidelines for the diagnosis and management of syncope. European Heart Journal (2009) 30, 2631-2671 doi:10.1093/eurheartj/ehp298 http://eurheartj.oxfordjournals.org/content/30/21/2631.full.pdf
(2) ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal (2011) 32, 2999-3054 doi:10.1093/eurheartj/ehr236
(3) ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal (2012) 33, 2569-2619 doi:10.1093/eurheartj/ehs215 http://eurheartj.oxfordjournals.org/content/33/20/2569.full.pdf
(4) Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. European Heart Journal (2013) 34, 2636-2648, doi:10.1093/eurheartj/eht210
(5) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. European Heart Journal (2012) 33, 1787-1847 doi:10.1093/eurheartj/ehs104.http://eurheartj.oxfordjournals.org/content/33/14/1787.full.pdf
Notes to editor
The ACCA Toolkit is available at the ESC Stand – ESC Plaza.
Authors: ESC Press Office
Tel: +34 670 521 210 (ESC Spokesperson Coordinator – Tanya Kenny)
Email: [email protected]
About the European Society of Cardiology
The European Society of Cardiology (ESC) represents more than 80 000 cardiology professionals across Europe and the Mediterranean. Its mission is to reduce the burden of cardiovascular disease in Europe.
About ESC Congress 2014
ESC Congress is currently the world’s largest international congress in cardiovascular medicine. ESC Congress 2014 takes place 30 August to 3 September at the Fira Gran Via congress centre in Barcelona, Spain.
About the Acute Cardiovascular Care Association (ACCA)
The Acute Cardiovascular Care Association (ACCA) is a registered branch of the ESC. Its aim is to improve the quality of care and outcomes of patients with acute cardiovascular diseases.
The press release has been approved by the Editor in Chief of the Toolkit.
###
“Junk” Blood Tests May Offer Life-Saving Information

|
Some 30 percent of all positive hospital blood culture samples are discarded every day because they’re “contaminated” - they reflect the presence of skin germs instead of specific disease-causing bacteria.
Rather than toss these compromised samples into the trash, clinicians may be able to use the resistance profiles of skin bacteria identified by these tests to treat patients with antibiotics appropriate to their ailment, Tel Aviv University researchers say. Dr. Gidi Stein and Dr. Danny Alon of TAU’s Sackler Faculty of Medicine and the Department of Internal Medicine B. at Beilinson Hospital, Rabin Medical Center, and Prof. Lilach Hadany and Uri Obolski of the Department of Molecular Biology and Ecology of Plants at TAU’s Faculty of Life Sciences conducted a retrospective study on more than 2,500 patients. Their test results demonstrate the unique diagnostic value of “erroneous” cultures.
The study showed the immediate effects on both public health questions and the treatment of individuals whose blood has been contaminated. The results were published in the Journal of Antimicrobial Chemotherapy.
Think before you toss
The more resistant the skin germs, the higher the risk of the infecting bacteria to be resistant, the researchers found. “These results can certainly be used for on-site clinical decisions. Once a contaminated sample has been found to be highly resistant, it is likely that the blood-borne pathogens will have a similar resistance pattern. Thus antibiotic treatment may be better targeted for the actual pathogens,” says Prof. Hadany.
In the study, the researchers processed the demographic information, hospital records, blood culture results, and date of death of all patients at the Rabin Medical Center with positive blood cultures from 2009-12. They found that out of 2,518 patients, 1,664 blood cultures drawn from 1,124 patients reflected the presence of a common skin contaminant, coagulase-negative staphylococci (CoNS). High overall CoNS resistance predicted high overall resistance of the bacteria causing disease or infection. Most importantly perhaps, highly resistant CoNS isolates were found to be associated with higher short-term mortality.
The researchers hope their conclusions will cause clinicians to pause before discarding contaminated blood test results.
 “Because we have found a direct correlation between resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated from the same patient, the results of these ‘junk’ samples can be used to predict patient mortality and correct empirical antibiotic therapy,” said Dr. Stein. “This should serve as an additional, non-invasive, diagnostic tool.”
“Because we have found a direct correlation between resistance profiles of CoNS contaminants and those of the actual infecting bacteria isolated from the same patient, the results of these ‘junk’ samples can be used to predict patient mortality and correct empirical antibiotic therapy,” said Dr. Stein. “This should serve as an additional, non-invasive, diagnostic tool.”
Public welfare
According to the researchers, most hospital patients are treated at the outset with broad spectrum antibiotics. Days later, after initial test results are known, clinicians replace broad spectrum antibiotics with more precise narrow-spectrum antibiotics, which treat the specific bacteria identified by the blood sample.
It is well known that narrow spectrum antibiotics are better for the body because they target specific bacteria as opposed to an entire microenvironment. Moreover, broad spectrum antibiotics might result in altered bacterial environments of the skin and gastro-intestinal tract, promoting inflammation and the emergence of resistant pathogens.
“The high rate of inappropriate antibiotic use puts patients and the general public at risk,” said Prof. Hadany. “Improved matching of the treatment to the needs of the patient might reduce antibiotic load and the emergence of resistance.”
###
American Friends of Tel Aviv University
Aspirin cuts risk of clots, DVT by a third - new study

|
Low dose aspirin lowers the occurrence of new venous blood clots - and represents a reasonable treatment option for patients who are not candidates for long-term anticoagulant drugs, such as warfarin, according to a new study published in today’s issue of Circulation.
“The study provides clear, consistent evidence that low-dose aspirin can help to prevent new venous blood clots and other cardiovascular events among people who are at risk because they have already suffered a blood clot,” says the study’s lead author, University of Sydney Professor, John Simes.
“The treatment effect of aspirin is less than can be achieved with warfarin or other new generation direct thrombin inhibitors, which can achieve more than an 80 per cent reduction in adverse circulatory and cardiopulmonary events.
“However, aspirin represents a useful treatment option for patients who are not candidates for anticoagulant drugs because of the expense or the increased risk of bleeding associated with anticoagulants.”
Key results
Compared to placebo patients, those who took 100mg daily of aspirin had a one-third reduction in the risk of:
thromboembolism, which is the obstruction of a blood vessel by a clot that has dislodged from another site in the circulation.
deep vein thrombosis (DVT), which is the formation of a blood clot in a deep vein, predominantly in the legs.
pulmonary embolism, which is a blood clot affecting the arteries that supply blood to the lungs.
myocardial infarction (heart attack), stroke or cardiovascular death.
Most people who have had a blood clot in a leg vein (deep-vein thrombosis) or an embolism (where the clot blocks the blood flow) have anticoagulant drug treatment (such as warfarin) for at least 6 months, first to dissolve the clot and then to prevent it happening again.
However, long-term anticoagulant drugs are expensive and inconvenient, requiring frequent regular blood tests and adjustments to the dosage. Further, there is an elevated risk that the treatment could cause bleeding in some patients. For people who are not able to cope with this, the viable alternative of taking regular aspirin will be a great benefit.
“The study provides evidence that after a first venous thrombosis or embolism, daily aspirin reduces the risk of another event, without causing undue bleeding. This treatment is an alternative to long-term anticoagulation and will be especially useful for patients who do not want the inconvenience of close medical monitoring or the risk of bleeding,” says Professor Simes.
“Aspirin will be ideal in the many countries where prolonged anticoagulant treatment is too expensive. A major benefit of this treatment is its cost-effectiveness. Aspirin is cheap, but it will save the treatment costs of the many recurrent clots that are prevented. This could mean a saving of millions of healthcare dollars worldwide.”
Co-investigator Tim Brighton, a senior haematologist at Sydney’s Prince of Wales Hospital, adds: “This important study demonstrates clearly that low-dose aspirin reduces the risks of further blood clot. This is especially important for patients who are not able to take long-term anticoagulant medications for whatever reason, such as personal preference, adverse effects of anticoagulant or cost.”
###
Fast facts
Deep-vein thrombosis (DVT) can occur during or after sedentary travel or other situations of inactivity or as a result of surgery.
The risk of DVT rises with smoking, overweight or high blood pressure.
A clot in a leg vein may be carried in the blood circulation to the lungs, causing pulmonary embolism. Sometimes a clot is unprovoked, as with the patients in the INSPIRE study, who did not have initial specific causes or risk factors.
The research collaboration combined the data from the Australia-led international ASPIRE study and the Italian WARFASA study. ASPIRE had 822 participants from Australia, New Zealand, Singapore, India and Argentina, followed up for an average of three years and WARFASA another 402 patients followed up for at least two years.
###
Dan Gaffney
[email protected]
61-481-004-782
University of Sydney
UNC Lineberger researchers develop new approach to identify ‘drivers’ of cancer

|
UNC Lineberger Comprehensive Cancer Center researchers have developed a new integrated approach to pinpoint the genetic “drivers” of cancer, uncovering eight genes that could be viable for targeted breast cancer therapy.
The study, published online August 24 in Nature Genetics, was authored by Michael Gatza, PhD, lead author and post-doctoral research associate; Grace Silva, graduate student; Joel Parker, PhD, director of bioinformatics, UNC Lineberger; Cheng Fan, research associate; and senior author Chuck Perou, PhD, professor of genetics and pathology.
These researchers studied a variety of cancer causing pathways, the step-by-step genetic alterations in which normal cells transition into cancerous cells, including the pathway that governs cancer cell growth rates. A high growth rate of cells, also known as cell proliferation, is recognized to be associated with poor prognosis for breast cancer patients.
Analyzing multiple types of genomic data, UNC Lineberger researchers were able to identify eight genes that were amplified on the genomic DNA level, and necessary for cell proliferation in luminal breast cancer, which is the most common sub-type of breast cancer.
“Using this new computational approach, we were able to take advantage of the rich data resources that exist and identify a number of new potential drug targets for a specific subset of breast cancer patients. This is an important step down the road towards more personalized medicine,” said Perou.
In fact, one of the genes identified – CPT1A – is already a target for drug development in lymphoma and could potentially be tested for breast cancer patients as well. Drugs targeting CPT1A have been shown to inhibit human cancer cell line growth in vitro and in mouse models of lymphoma.
This analytical approach used to better understand the drivers of cancers includes a comprehensive and integrated analysis of multiple data types including gene expression data, somatic mutations, DNA copy number, and a functional genomics data set.
While the study focused on identifying genetic drivers for breast cancer, the approach could easily be applied to other tumors types as well. Lead author Mike Gatza added, “While we were able to pinpoint drivers for breast cancer, this approach can and will be applied to other tumor types in the future.”
###
About UNC Lineberger
One of only 41 NCI-designated comprehensive cancer centers, the University of North Carolina Lineberger Comprehensive Cancer Center brings together some of the most exceptional physicians and scientists in the country to investigate and improve the prevention, early detection and treatment of cancer. With research that spans the spectrum from the laboratory to the bedside to the community, UNC Lineberger faculty work to understand the causes of cancer at the genetic and environmental levels, to conduct groundbreaking laboratory research, and to translate findings into pioneering and innovative clinical trials. For more information, please visit http://www.unclineberger.org.
Media Contact: Katy Jones, UNC Lineberger Comprehensive Cancer Center’s Director of Communications and Marketing, at [email protected] or 919-883-7848.
###
Katy Jones
[email protected]
919-883-7848
University of North Carolina Health Care
Train your heart to protect your mind

|
Exercising to improve our cardiovascular strength may protect us from cognitive impairment as we age, according to a new study by researchers at the University of Montreal and its affiliated Institut universitaire de gératrie de Montréal Research Centre. “Our body’s arteries stiffen with age, and the vessel hardening is believed to begin in the aorta, the main vessel coming out of the heart, before reaching the brain. Indeed, the hardening may contribute to cognitive changes that occur during a similar time frame,” explained Claudine Gauthier, first author of the study. “We found that older adults whose aortas were in a better condition and who had greater aerobic fitness performed better on a cognitive test. We therefore think that the preservation of vessel elasticity may be one of the mechanisms that enables exercise to slow cognitive aging.”
The researchers worked with 31 young people between the ages of 18 and 30 and 54 older participants aged between 55 and 75. This enabled the team to compare the older participants within their peer group and against the younger group who obviously have not begun the aging processes in question. None of the participants had physical or mental health issues that might influence the study outcome. Their fitness was tested by exhausting the participants on a workout machine and determining their maximum oxygen intake over a 30 second period. Their cognitive abilities were assessed with the Stroop task. The Stroop task is a scientifically validated test that involves asking someone to identify the ink colour of a colour word that is printed in a different colour (e.g. the word red could be printed in blue ink and the correct answer would be blue). A person who is able to correctly name the colour of the word without being distracted by the reflex to read it has greater cognitive agility.
The participants undertook three MRI scans: one to evaluate the blood flow to the brain, one to measure their brain activity as they performed the Stroop task, and one to actually look at the physical state of their aorta.
The researchers were interested in the brain’s blood flow, as poorer cardiovascular health is associated with a faster pulse wave,at each heartbeat which in turn could cause damage to the brain’s smaller blood vessels. “This is first study to use MRI to examine participants in this way,” Gauthier said. “It enabled us to find even subtle effects in this healthy population, which suggests that other researchers could adapt our test to study vascular-cognitive associations within less healthy and clinical populations.”
The results demonstrated age-related declines in executive function, aortic elasticity and cardiorespiratory fitness, a link between vascular health and brain function, and a positive association between aerobic fitness and brain function. “The link between fitness and brain function may be mediated through preserved cerebrovascular reactivity in periventricular watershed areas that are also associated with cardiorespiratory fitness,” Gauthier said. “Although the impact of fitness on cerebral vasculature may however involve other, more complex mechanisms, overall these results support the hypothesis that lifestyle helps maintain the elasticity of arteries, thereby preventing downstream cerebrovascular damage and resulting in preserved cognitive abilities in later life.”
###
About this Study
This work was supported by the Canadian Institutes for Health Research (MOP 84378, Banting and Best Scholarship held by CJG, Canadian Research Chair to LB), the Canadian Foundation for Innovation (Leaders Opportunity Fund 17380), the Ministère du développement économique, de l’innovation et de l’exportation (PSR-SIIRI-239) and the Canadian National Sciences and Engineering Research Council (R0018142). The findings were published in Neurobiology of Aging on August 20, 2014. The University of Montreal is officially known as Université de Montréal.
###
William Raillant-Clark
[email protected]
514-566-3813
University of Montreal
New enzyme targets for selective cancer therapies

|
Thanks to important discoveries in basic and clinical research and technological advances, the fight against cancer has mobilized into a complex offensive spanning multiple fronts.
Work happening in a University of Alberta chemistry lab could help find new and more selective therapies for cancer. Researchers have developed a compound that targets a specific enzyme overexpressed in certain cancers - and they have tested its activity in cells from brain tumours.
Chemistry professor Christopher Cairo and his team synthesized a first-of-its-kind inhibitor that prevents the activity of an enzyme called neuraminidase. Although flu viruses use enzymes with the same mechanism as part of the process of infection, human cells use their own forms of the enzyme in many biological processes.
Cairo’s group collaborated with a group in Milan, Italy, that has shown that neuraminidases are found in excess amounts in glioblastoma cells, a form of brain cancer.
In a new study, a team from the University of Milan tested Cairo’s enzyme inhibitor and found that it turned glioblastoma cancer stem cells - found within a tumour and believed to drive cancer growth - into normal cells. The compound also caused the cells to stop growing, suggesting that this mechanism could be important for therapeutics. Results of their efforts were published Aug. 22 in the Nature journal Cell Death & Disease.
Cairo said these findings establish that an inhibitor of this enzyme could work therapeutically and should open the door for future research.
 “This is the first proof-of-concept showing a selective neuraminidase inhibitor can have a real effect in human cancer cells,” he said. “It isn’t a drug yet, but it establishes a new target that we think can be used for creating new, more selective drugs.”
“This is the first proof-of-concept showing a selective neuraminidase inhibitor can have a real effect in human cancer cells,” he said. “It isn’t a drug yet, but it establishes a new target that we think can be used for creating new, more selective drugs.”
Long road from proof of concept to drug
Proving the compound can successfully inhibit the neuraminidase enzyme in cancer cells is just the first step in determining its potential as a therapy.
In its current form, the compound could not be used as a drug, Cairo explained, largely because it wasn’t designed to breach the blood-brain barrier making it difficult to reach the target cells. The team in Milan had to use the compound in very high concentrations, he added.
The research advances our understanding of how important carbohydrates are to the function of cells. Although most of us think of glucose (blood sugar) as the only important sugar in biology, there is an entire area of research known as glycobiology that seeks to understand the function of complex carbohydrate structures in cells. Carbohydrate structures cover the surface of cells, and affect how cells interact with each other and with pathogens.
Scientists have known for decades that the carbohydrates found on cancer cells are very different from those on normal cells. For example, many cancers have different amounts of specific residues like sialic acid, or may have different arrangements of the same residues.
“The carbohydrates on the cell surface determine how it interacts with other cells, which makes them important in cancer and other diseases. So, if we can design compounds that change these structures in a defined way, we can affect those interactions,” Cairo explained. “Finding new enzyme targets is essential to that process, and our work shows that we can selectively target this neuraminidase enzyme.”
Although there has been a lot of work on targeting viral neuraminidase enzymes, Cairo’s team has found inhibitors of the human enzymes. “The challenge in human cells is that there are four different isoenzymes. While we might want to target one for its role in cancer, hitting the wrong one could have harmful side-effects,” he said.
The U of A team reached out to their colleagues in Milan who were studying the role of a specific neuraminidase isoenzyme in cancer cells isolated from patients. Cairo approached them about testing a compound his team identified last year, which was selective for the same isoenzyme.
“I expected it would do something, but I didn’t know it would be that striking. It came out beautifully,” Cairo said.
The U of A team is already working on improving the compound, and developing and testing new and existing inhibitors using a panel of in vitro assays they developed.
“We’ve been working on these enzymes for about five years. Validation of our strategy-design of a selective neuraminidase inhibitor and application in a cell that overexpresses that enzyme - is an achievement for us.”
The U of A’s team was funded by the Alberta Glycomics Centre, the Cancer Research Society and the Natural Sciences and Engineering Research Council of Canada.
###
By Bryan Alary
University of Alberta 116 St. and 85 Ave., Edmonton, AB, Canada T6G 2R3
Offering option of initial HIV care at home increases use of ART

|
LSTM Researchers found that offering adults in Malawi optional home initiation of care following HIV self-testing resulted in a significant increase in the proportion of adults initiating antiretroviral therapy compared with standard HIV care
LSTM Researchers found that offering adults in Malawi optional home initiation of care following HIV self-testing resulted in a significant increase in the proportion of adults initiating antiretroviral therapy (ART) compared with standard HIV care.
The results are part of a study that was funded by the Wellcome Trust and published in the July 23/30 issue of JAMA, which is HIV/AIDS themed and released early to coincide with the International AIDS Conference taking place in Melbourne, Australia next week.
In 2012 it was estimated that 35 million people worldwide were living with the human immunodeficiency virus (HIV). ART not only substantially reduces the risk of HIV transmission but also greatly reduces illness and death, which raises hopes that a high uptake of annual HIV testing and early initiation of ART could improve HIV prevention as well as care.
HIV self-testing, where an individual performs and interprets their own HIV test in private, is a novel approach that has been high acceptability in Malawi and the United States. HIV self-testing can overcome barriers to conventional facility- and community-based testing that lack privacy and convenience.
Dr Peter MacPherson of LSTM and the Malawi-Liverpool-Wellcome Trust Clinical Research Programme, and colleagues, recruited 16,660 adult residents of Blantyre, Malawi, where nearly one in five adults are infected with HIV. Participants received access to HIV self-testing through community volunteers and were randomised to receive either facility-based HIV care, or optional home initiation of HIV care following reporting of a positive HIV self-test result.
During the six months of availability, 58% of all adult participants took an HIV self-test kit. A significantly greater proportion of adults in the home group initiated ART (181/8,194; 2.2%) compared with the facility group (63/8,466; 0.7%). Participants in the home group (6.0%) were also significantly more likely to report a positive HIV self-test result to counsellors than facility group participants (3.3%).
Dr MacPherson said: “These results are extremely encouraging. Our study found that population-level ART initiations were increased by the availability of home initiation of care. We know that early uptake of ART can help prevent HIV infections, as well as dramatically improve health”.
“At a time when universal test and treat approaches to controlling the HIV epidemic are being considered, home initiation of HIV care shows high promise as a simple strategy to improve the uptake of ART when HIV self-testing is carried out at home.”
###
Clare Bebb
[email protected]
44-015-170-53135
Liverpool School of Tropical Medicine
Sleep Loss Accelerates Brain Aging: Study

|
Getting a good night’s sleep may help you stay sharp mentally as you age, a new study suggests.
Researchers at Duke-NUS Graduate Medical School Singapore have found that the less seniors sleep, the faster their brains age. These findings suggest sleep deprivation is a significant factor in cognitive decline, including dementia.
Past studies have demonstrated that sleep quality and duration can affect the cognitive functions of older adults, but the latest study suggests why.
The Duke-NUS study examined tracked 66 older Chinese adults, who underwent structural MRI brain scans measuring brain volume and tests of cognitive function every two years. Researchers also asked the seniors how well - and how long - they slept each night.
The results showed those who reported sleeping fewer hours had distinctly different brain features that have been linked to age-related cognitive decline and the development of neurodegenerative diseases such as Alzheimer’s - specifically: faster ventricle enlargement - than those who slept more hours.
“Our findings relate short sleep to a marker of brain aging,” said lead researcher June Lo, M.D. “Work done elsewhere suggests that seven hours a day for adults seems to be the sweet spot for optimal performance on computer based cognitive tests. In coming years we hope to determine what’s good for cardio-metabolic and long term brain health too.”
The study was published in the journal Sleep.
###
NewsmaxHealth
To advance care for patients with brain metastases: Reject five myths

|
A blue-ribbon team of national experts on brain cancer says that professional pessimism and out-of-date “myths,” rather than current science, are guiding - and compromising - the care of patients with cancers that spread to the brain.
In a special article published in the July issue of Neurosurgery, the team, led by an NYU Langone Medical Center neurosurgeon, argues that many past, key clinical trials were designed with out-of-date assumptions and the tendency of some physicians to “lump together” brain metastases of diverse kinds of cancer, often results in less than optimal care for individual patients. Furthermore, payers question the best care when it deviates from these misconceptions, the authors conclude.
“It’s time to abandon this unjustifiable nihilism and think carefully about more individualized care,” says lead author of the article, Douglas S. Kondziolka, M.D., MSc, FRCSC, Vice Chair of Clinical Research and Director of the Gamma Knife Program in the Department of Neurosurgery at NYU Langone. The authors - who also say medical insurers help perpetuate the myths by denying coverage that deviates from them - identify five leading misconceptions that often lead to poorer care:
1. All tumor cell types act the same way once they spread to the brain. This oversimplification means that doctors assume that histologically diverse cancers respond the same way to chemotherapy and are equally sensitive (or insensitive) to radiation. It also means that patients are all assumed to be at the same risk of subsequent brain cancer relapses, and development of additional metastatic lesions; and that survival rates are similar as well. The authors point out that this type of thinking overlooks important biological differences in brain metastases resulting from different types of cancer, such as those originating in the lung, breast or skin.
2. The number of brain metastases is the best indicator for guiding management of the disease. Such strict adherence to quantity, the authors say, can wrongly limit treatment options. Physicians should look at total tumor burden, including the size and scope of metastases, rather than just how many metastases occur.
 3. All cancers detectable in the brain already reflect the presence of micrometastases, or smaller, newly formed tumors too miniscule to detect. Evidence, the authors say, suggests otherwise, and aggressively monitoring for, and treating, individual brain metastases can, in fact, improve tumor control and patient survival.
3. All cancers detectable in the brain already reflect the presence of micrometastases, or smaller, newly formed tumors too miniscule to detect. Evidence, the authors say, suggests otherwise, and aggressively monitoring for, and treating, individual brain metastases can, in fact, improve tumor control and patient survival.
4. Whole brain radiation (WBR) is generally unjustified because it will cause disabling cognitive dysfunction if a patient lives long enough. Dr. Kondziolka and his co-authors say the risks and benefits of WBR should be evaluated for each patient, and that new studies examining the cognitive impact of WBR on thinking and learning are underway.
5. Most brain metastases cause obvious symptoms, making regular screening for them unnecessary, and unlikely to affect survival. The authors counter that advances in screening allow metastases to be detected earlier, and treated sooner, before symptoms occur.
“We are in an era of personalized medicine,” Dr. Kondziolka says, “and we need to begin thinking that way.” The authors further write: “It is time for fresh thinking and new critical analyses,” urging consideration of updated clinical trial designs that include comparison of matched cohorts and cost effectiveness factors. In addition to research that pays more attention to specific cell types and overall tumor burden, investigators should focus on tools available from advances in molecular biology and genetic subtyping and on efforts to learn “why some patients with a given primary cancer develop brain tumors and others do not.” Ultimately, the authors hope better stratifying patients will improve care for patients with diverse brain metastases.
###
In addition to Dr. Kondziolka from NYU Langone Medical Center, the co-authors represent other major academic medical centers with national reputations in the field of neurosurgery, radiation oncology and neuro-oncology: Steven Kalkanis, MD (Henry Ford Health System), Minesh Mehta, MD (University of Maryland Medical Center), Manmeet Ahluwalia, MD (Cleveland Clinic) and Jay Loeffler, MD (Harvard Medical School).
About NYU Langone Medical Center:
NYU Langone Medical Center, a world-class, patient-centered, integrated academic medical center, is one of the nation’s premier centers for excellence in clinical care, biomedical research, and medical education. Located in the heart of Manhattan, NYU Langone is composed of four hospitals - Tisch Hospital, its flagship acute care facility; Rusk Rehabilitation; the Hospital for Joint Diseases, the Medical Center’s dedicated inpatient orthopaedic hospital; and Hassenfeld Pediatric Center, a comprehensive pediatric hospital supporting a full array of children’s health services across the Medical Center - plus the NYU School of Medicine, which since 1841 has trained thousands of physicians and scientists who have helped to shape the course of medical history. The Medical Center’s tri-fold mission to serve, teach, and discover is achieved 365 days a year through the seamless integration of a culture devoted to excellence in patient care, education, and research.
###
Poor quality of life may affect teens’ diabetes management
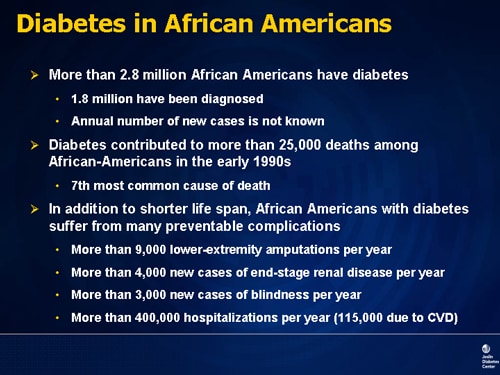
|
In the years after being diagnosed with diabetes, adolescents struggling with social and psychological burdens of managing the disease are likely to do a worse job of controlling it, according to a new U.S. study.
Teens who reported a lower quality of life were more likely to have rising levels of hemoglobin A1c, a marker of elevated blood sugar over time and a sign of poor diabetes control.
“We need to intervene from a prevention standpoint,” said Korey Hood, a psychologist at the University of California, San Francisco and lead author of the study. “We need to do systematic screening of these psychosocial issues.”
Teens who are psychologically stressed are less likely to take care of themselves, which could explain the rise in A1c levels, added Michael Scharf, a psychiatrist at the University of Rochester Medical Center who was not involved in the study.
By catching the problem early, it might be possible to keep the disease from getting worse, he told Reuters Health.
“When I see them, people are stressed out by how sick they are,” Scharf said. “The sad part is that if we could have intervened earlier we may have been able to help prevent the negative medical consequences of poorly controlled diabetes.”
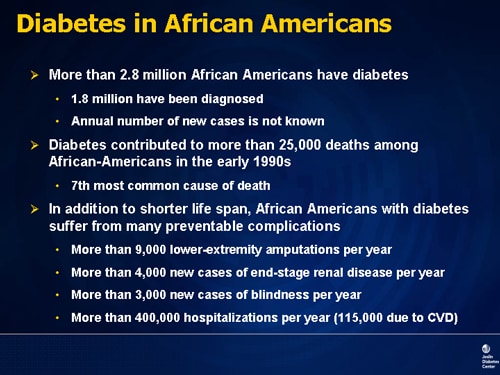 The new study followed youth with either type 1 or type 2 diabetes for about six years from the time they were diagnosed. Type 1 diabetes, formerly known as juvenile diabetes, typically appears in childhood or adolescence and results from a failure to make insulin, a hormone that helps the body use blood sugar for energy.
The new study followed youth with either type 1 or type 2 diabetes for about six years from the time they were diagnosed. Type 1 diabetes, formerly known as juvenile diabetes, typically appears in childhood or adolescence and results from a failure to make insulin, a hormone that helps the body use blood sugar for energy.
Type 2 diabetes, more commonly seen in adults and often linked to obesity, happens when the body makes insulin but is unable to use it. Over time, too much sugar in the blood can cause damage to the eyes, kidneys and to nerves throughout the body. Too little blood sugar can lead to coma.
Altogether, about 151,000 people younger than 20 years old in the U.S. have diabetes, according to the Centers for Disease Control and Prevention. Out of the general population in 2009, 19 kids per 10,000 had type 1 diabetes and 3 per 10,000 had type 2 diabetes.
Managing the disease is similar for kids with type 1 and type 2, and particularly in type 1 it involves taking insulin daily to keep blood sugar levels steady. For kids with type 2 disease, there’s more focus on diet, exercise and medications, according to Hood and his coauthors.
Past research has shown that young people with diabetes are more prone than their peers without the disease to experience psychosocial difficulties in general and depression in particular. Hood and his colleagues wanted to find out if those problems affected the teens’ ability to manage their blood sugar.
 They analyzed medical records and interviews for 1,307 kids who were over age 10 at the beginning of the study period and had been diagnosed within the previous year. The researchers then followed the childrens’ mental and physical health, looking for connections between the two.
They analyzed medical records and interviews for 1,307 kids who were over age 10 at the beginning of the study period and had been diagnosed within the previous year. The researchers then followed the childrens’ mental and physical health, looking for connections between the two.
Across the entire group, A1c levels rose by about 1.5 percent over the study period.
Among the teens who reported poor quality of life related to their disease - such as diabetes causing difficulties with their social life or school performance - A1c levels tended to run higher than in kids without quality of life issues.
A1c was also higher among kids whose quality of life worsened from the start of the study period to the end, according to the findings published in the Journal of Adolescent Health.
Teens with type 2 diabetes tended to be worse off in general, reporting more mental health issues, including depression, and a lower quality of life than the kids with type 1 disease, the researchers note.
The constant presence of health problems could isolate teens from their peers and make them feel frustrated, said Ingrid Libman, a pediatric endocrinologist at the Children’s Hospital of Pittsburgh.
However, the mental health differences could also be caused by outside stress. Adolescents with type 2 diabetes are often born into families who are poor and don’t have insurance. Either way, Hood said, teens and their relatives could benefit from counseling.
“I hope that a study like this can help raise awareness that monitoring a patient and a family’s stress level should really be part of care before it becomes a problem,” Scharf said.
Hood and his team say doctors should talk to teens about their quality of life and mental health issues at every check up.
SOURCE: Journal of Adolescent Health, online May 12, 2014
###
Psychosocial Burden and Glycemic Control During the First 6 Years of Diabetes: Results From the SEARCH for Diabetes in Youth Study
Purpose
To evaluate the psychosocial burden of adolescents with diabetes, determine the trajectory of psychosocial burden, and examine the interdependent relationships between psychosocial burden and glycemic control across the first 6 years of diabetes.
Methods
Data from SEARCH for Diabetes in Youth, an observational study of U.S. children diagnosed with diabetes before the age of 20, were collected during study visits conducted at baseline and then at 12, 24, and 60 months after baseline. Blood was drawn, clinical and demographic information was collected, and psychosocial burden was evaluated using standardized depression and generic and diabetes-specific health-related quality of life (QOL) surveys.
Results
Among the 1,307 adolescents (mean age, 14.1±2.5 years) with baseline data, 1,026 had type 1 diabetes and 281 had type 2 diabetes. For those with a 60-month follow-up visit, glycated hemoglobin (A1c) values rose 1.5% from baseline (type 1, 7.7%–9.3% and type 2, 7.3%–8.8%). Adolescents with type 2 diabetes reported more depression and poorer QOL than adolescents with type 1 diabetes. For each diabetes type, there were similar baseline risk factors for higher A1c values: longer diabetes duration, ethnic minority status, and declining diabetes QOL (p
< .05). However, youth with type 2 diabetes had higher A1c values with increasing generic QOL, an unexpected finding. Younger adolescents with type 1 diabetes had higher A1c values at the end of the study.
Conclusions
Significant deterioration in glycemic control marks the first 6 years of diabetes for adolescents. Psychosocial burden, particularly poor diabetes-specific QOL, is a contributor to suboptimal glycemic outcomes.
Korey K. Hood, Ph.D.,
Daniel P. Beavers, Ph.D.,
Joyce Yi-Frazier, Ph.D.,
Ronny Bell, Ph.D.,
Dana Dabelea, M.D., Ph.D.,
Robert E. Mckeown, Ph.D.,
Jean M. Lawrence, Sc.D., M.P.H., M.S.S.A.
Study Explains How High Blood Pressure in Middle Age Affects Memory in Old Age

|
High blood pressure in middle age plays a critical role in whether blood pressure in old age may affect memory and thinking, according to a study published in the online edition of the journal Neurology.
“Our findings bring new insight into the relationship between a history of high blood pressure, blood pressure in old age, the effects of blood pressure on brain structure, and memory and thinking,” said study author Lenore J. Launer, PhD, National Institute on Aging, part of the National Institutes of Health (NIH), Bethesda, Maryland.
For the study, 4,057 older participants free of dementia had their blood pressure measured in middle-age (mean age, 50 years). In late life (mean age, 76 years) their blood pressure was re-measured and participants underwent magnetic resonance imaging (MRI) scans that looked at structure and damage to the small vessels in the brain. They also took tests that measured their memory and thinking ability.
The study found that the association of blood pressure in old age to brain measures depended on a history of blood pressure in middle age. Higher systolic and diastolic blood pressure was associated with increased risk of brain lesions and tiny brain bleeds. This was most noticeable in people without a history of high blood pressure in middle age. For example, people with no history of high blood pressure in middle age who had high diastolic blood pressure in old age were 50% more likely to have severe brain lesions than people with low diastolic blood pressure in old age.
However, in people with a history of high blood pressure in middle age, lower diastolic blood pressure in older age was associated with smaller total brain and gray matter volumes. This finding was reflected in memory and thinking performance measures as well. In people with high blood pressure in middle age, lower diastolic blood pressure was associated with 10% lower memory scores.
“Older people without a history of high blood pressure but who currently have high blood pressure are at an increased risk for brain lesions, suggesting that lowering of blood pressure in these participants might be beneficial,” said Dr. Launer. “On the other hand, older people with a history of high blood pressure but who currently have lower blood pressure might have more extensive organ damage and are at risk of brain shrinkage and memory and thinking problems.”
###
SOURCE: American Academy of Neurology
Climate engineering can’t erase climate change

|
Tinkering with climate change through climate engineering isn’t going to help us get around what we have to do says a new report authored by researchers at six universities, including Simon Fraser University.
After evaluating a range of possible climate-altering approaches to dissipating greenhouse gases and reducing warming, the interdisciplinary team concluded there’s no way around it. We have to reduce the amount of carbon being released into the atmosphere.
“Some climate engineering strategies look very cheap on paper. But when you consider other criteria, like ecological risk, public perceptions and the abilities of governments to control the technology, some options look very bad,” says Jonn Axsen.
The assistant professor in SFU’s School of Resource and Environmental Management is a co-author on this study, which appears in the latest issue of the peer-reviewed journal Frontiers in Ecology and the Environment. It is the first scholarly attempt to rank a wide range of approaches to minimizing climate change in terms of their feasibility, cost-effectiveness, risk, public acceptance, governability and ethics.
It states reducing emissions, through some combination of switching away from fossil fuels to low-carbon energy sources, improving energy efficiency, and changing human behaviour, is still the most effective way of confronting climate change.
The authors note though that some approaches to climate engineering are more promising than others, and they should be used to augment efforts to reduce the climate-change effects resulting from human activity. For example, strategies such as forest management and geological storage of carbon dioxide may be useful complements.
Other climate engineering strategies are less appealing, such as fertilizing the ocean with iron to absorb carbon dioxide or reducing global warming by injecting particles into the atmosphere to block sunlight.
“Take the example of solar radiation management, which is the idea of putting aerosols into the stratosphere, kind of like what happens when a large volcano erupts,” Axsen explains.
“This is a surprisingly cheap way to reduce global temperatures, and we have the technology to do it. But our study asked other important questions. What are the environmental risks? Will global citizens accept this? What country would manage this? Is that fair? Suddenly, this strategy does not look so attractive.”
Working under the auspices of the National Science Foundation, the authors spent two years evaluating more than 100 studies that addressed the various implications of climate engineering and their anticipated effects on greenhouse gases.
The authors hope their study will help the public and decision-makers invest in the approaches with the largest payoffs and the fewest disadvantages. At stake, they emphasize, are the futures of our food production, climate and water security.
###
Background: Axsen’s collaborators were Daniela Cusack, an assistant professor of geography in the University of California, Los Angeles’ College of Letters and Science; Lauren Hartzell-Nichols, acting assistant professor in The Program on Values in Society and The Program on Environment at the University of Washington; Katherine Mackey, a postdoctoral researcher at Woods Hole Oceanographic Institution and the Marine Biological Laboratory; Rachael Shwom, assistant professor in human ecology at Rutgers University; and Sam White, assistant professor of environmental history at Ohio State University.
Simon Fraser University is consistently ranked among Canada’s top comprehensive universities and is one of the top 50 universities in the world under 50 years old. With campuses in Vancouver, Burnaby and Surrey, B.C., SFU engages actively with the community in its research and teaching, delivers almost 150 programs to more than 30,000 students, and has more than 125,000 alumni in 130 countries.
Simon Fraser University: Engaging Students. Engaging Research. Engaging Communities.
Contact: Jonn Axsen, 778.782.9365, 778.239.1169, [email protected]
Carol Thorbes, PAMR, 778.782.3035, [email protected]
Note: Axsen will be available to do media interviews starting at 11 a.m., Tuesday, June 2.
###
Carol Thorbes
[email protected]
778-782-3035
Simon Fraser University
Experts recommend blood, urine testing to diagnose rare adrenal tumors

|
The Endocrine Society today issued a Clinical Practice Guideline (CPG) for the diagnosis and treatment of two types of rare adrenal tumors - pheochromocytomas and paragangliomas - that can raise the risk of cardiovascular disease and even death if left untreated.
The CPG, entitled “Pheochromocytoma and Paraganglioma: An Endocrine Society Clinical Practice Guideline,” appeared in the June 2014 issue of the Journal of Clinical Endocrinology and Metabolism (JCEM), a publication of the Endocrine Society.
Pheochromocytomas are rare, usually noncancerous tumors that form inside the adrenal glands, while paragangliomas are similar tumors that develop outside the glands. The tumors cause the body to produce excess amounts of the hormones epinephrine - commonly known as adrenaline - and norepinephrine, which is involved in regulating blood pressure. Symptoms of these tumors include high blood pressure, episodic severe headaches, excess sweating, racing heart, feelings of anxiety and trembling.
Experts estimate between 0.1 and 1 percent of patients treated for high blood pressure have pheochromocytomas, according to the National Institutes of Health’s National Cancer Institute.
“Correctly diagnosing pheochromocytomas and paragangliomas is extremely important,” said Jacques W.M. Lenders, MD, PhD, FRCP, of Radboud University in Nijmegen, the Netherlands, and chair of the task force that authored the guideline. “In addition to the strain these tumors put on the cardiovascular system, between 10 and 17 percent of the tumors can become malignant. Researchers have discovered that at least a third of people with these conditions have a disease-causing genetic mutation, so early detection can benefit family members who may be at risk.”
In the CPG, the Endocrine Society recommends that initial testing for pheochromocytomas and paragangliomas include blood or urine tests for metanephrines - the products left behind when the body metabolizes epinephrine and norepinephrine. Research has shown blood and urine testing for metanephrines are more effective at identifying patients who have pheochromocytomas or paragangliomas than other testing techniques.
About the adrenal glands
The adrenals are small glands that sit above each of the kidneys. The kidneys are located deep inside the upper part of the abdomen.
The adrenal gland has 2 parts. The outer part, called the cortex, is where most tumors develop. The function of the cortex is to make certain hormones for the body. These hormones all have a similar chemical structure and are called steroids. They include:
Cortisol causes changes in metabolism that help the body to handle stress.
Aldosterone helps the kidneys regulate the amount of salt in the blood and helps regulate blood pressure.
Adrenal androgens are hormones which can be converted to more common forms of the sex hormones estrogen and testosterone in other parts of the body. The amount of these hormones that result from conversion of adrenal androgens is small compared to what is made in other parts of the body. The testicles produce most of the androgens (male hormones) in men. The ovaries produce most of the estrogens (female hormones) in women.
Other recommendations from the CPG include:
People who are diagnosed with pheochromocytomas or paragangliomas should be involved in a shared decision-making process with their physicians to evaluate the need for genetic testing;
A diagnostic algorithm that takes into account risk factors such as age at tumor presentation and family history should be used to establish which patients would benefit most from genetic testing and which specific gene mutations to test for;
People with paragangliomas and those diagnosed with metastatic tumors should be tested for specific gene mutations associated with those conditions;
Computed tomography can be used as the first choice imaging technology for determining the location of pheochromocytomas or paragangliomas for surgical treatment;
MRI imaging technology is to be used in specific situations, including for patients who have metastatic tumors, for detecting head and neck paragangliomas and for patients in whom radiation exposure should be limited; and
Another imaging technology, 18F-fluorodeoxyglucose-positron emission tomography/computed tomography, can be used in patients with metastatic tumors.
Other members of the Endocrine Society task force that developed this CPG include: Quan-Yang Duh of the VA Medical Center and University of California, San Francisco; Graeme Eisenhofer of the University Hospital Dresden in Dresden, Germany; Anne-Paule Gimenez-Roqueplo of Assistance Publique-Hôpitaux de Paris, Hôpital Européen Georges Pompidou and Université Paris Descartes in Paris, France; Stefan K.G. Grebe, Mohammad Hassan Murad and William F. Young, Jr. of the Mayo Clinic in Rochester, MN; Mitsuhide Naruse of National Hospital Organisation Kyoto Medical Center in Kyoto, Japan; and Karel Pacak of the Eunice Kennedy Shriver National Institute of Child Health & Human Development in Bethesda, MD.
Types of adrenal gland tumors
A tumor begins when normal cells change and grow uncontrollably, forming a mass. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can spread to other parts of the body. A benign tumor means the tumor will not spread.
A tumor can start in an adrenal gland, called a primary adrenal tumor, or it can begin in another organ, such as the lungs, and then spread to the adrenal glands. An adrenal gland tumor can sometimes overproduce hormones. When it does, the tumor is called a functioning tumor. An adrenal gland tumor that does not produce hormones is called a nonfunctioning tumor. The symptoms and treatment of an adrenal gland tumor depend on whether the tumor is functioning or nonfunctioning, what hormone(s) is overproduced, and whether the tumor is a primary adrenal gland tumor or if the cancer has spread from another organ.
This section focuses on primary adrenal gland tumors, which include the following:
Adenoma. Also called an adrenocortical adenoma, this is the most common type of adrenal gland tumor. It is a noncancerous, nonfunctioning tumor of the adrenal cortex. An adenoma usually does not cause symptoms and, if it is small, often does not need treatment.
Adrenocortical carcinoma. Although rare, adrenocortical carcinoma is the most common type of cancerous adrenal gland tumor. It is also known as adrenal cortical carcinoma. Approximately four to 12 out of one million people develop this type of tumor, which begins in the adrenal cortex. Adrenocortical carcinoma can be a functioning or nonfunctioning tumor. If the tumor is functioning, it may produce more than one hormone.
Neuroblastoma. This is a type of childhood cancer that can begin in the adrenal medulla. Learn more about childhood neuroblastoma.
Pheochromocytoma. This type of neuroendocrine tumor most often begins in the adrenal medulla. Learn more about pheochromocytoma.

The Society established the CPG Program to provide endocrinologists and other clinicians with evidence-based recommendations in the diagnosis and treatment of endocrine-related conditions. Each CPG is created by a task force of topic-related experts in the field. Task forces rely on scientific reviews of the literature in the development of CPG recommendations. The Endocrine Society does not solicit or accept corporate support for its CPGs. All CPGs are supported entirely by Society funds.
The CPG was co-sponsored by the American Association for Clinical Chemistry and the European Society of Endocrinology.
###
Founded in 1916, the Endocrine Society is the world’s oldest, largest and most active organization devoted to research on hormones and the clinical practice of endocrinology. Today, the Endocrine Society’s membership consists of over 17,000 scientists, physicians, educators, nurses and students in more than 100 countries. Society members represent all basic, applied and clinical interests in endocrinology. The Endocrine Society is based in Washington, DC.
###
Jenni Glenn Gingery
[email protected]
202-971-3655
The Endocrine Society
Stopping statins may benefit terminally ill patients

|
People in the late stages of cancer and other terminal illnesses are not only unharmed by discontinuing statins for cholesterol management, they may benefit, according to a study presented Friday by researchers at Duke Medicine representing a national research network.
The finding addresses a thorny question in treating people with life-limiting illnesses: When, if ever, is it appropriate to discontinue medications prescribed for other conditions that will likely not lead to their death?
In an analysis presented at the American Society of Clinical Oncology annual meeting in Chicago, the researchers reported that discontinuing statins in patients with advanced illnesses resulted in improved overall quality of life, lower costs and no increased deaths. In fact, the patients who stopped taking statins appeared to live slightly longer.
“When you look at the number of medications people take when they are dying, it doubles in the last year of life,” said lead author Amy Abernethy, M.D., Ph.D., director of the Center for Learning Health Care at the Duke Clinical Research Institute and a member of the Duke Cancer Institute. Abernethy represented the Palliative Care Research Cooperative Group, a national research network focused on improving care for people with serious illnesses.
“Cancer patients, for example, take medications for pain, nausea and other problems associated with advanced disease,” Abernethy said. “Many don’t have an appetite, and simply swallowing medications can be a problem. So the issue is whether some longstanding medications such as cholesterol-lowering drugs might be safely discontinued, but there has been little research to help guide clinicians in making that recommendation.”
Abernethy said the researchers identified statins as a good candidate to explore the issue, because the drug is widely prescribed and benefits can take years to accrue. Other drugs the researchers could eventually study include medications for blood pressure and blood clots.
In their study of statins, Abernethy and colleagues enrolled 381 patients who faced the likelihood of dying within a year. All patients had been taking statins for at least three months; roughly half were randomized to continue taking the drug, the other half to discontinuing it.
The researchers followed the patients for up to a year to monitor survival, cardiovascular events and changes in quality of life.
Among the 192 study patients who continued statins, the median survival was 190 days; the 192 participants who stopped taking the drugs had a median survival of 229 days.
Those who discontinued the drugs reported a better overall quality of life, particularly in their psychological wellbeing, and saved money: $716 per person over the course of the trial for name-brand drugs, and $629 for generics.
Using U.S. population estimates, the researchers reported that as much as $603 million a year could be saved if patients in the late stages of fatal illnesses were to cut out statins.
“This is a decision that needs to be discussed between patients and their doctors; it’s not something that should be done independently or in a one-size-fits-all manner,” Abernethy said. “But our study found that patients who discontinued statins reported improvements in quality of life. This runs counter to the idea that discontinuing a treatment would cause people to somehow feel as if they were getting less care or inadequate care.”
Abernethy is a leading advocate for extending palliative care—extra support from care teams to relieve both pain and improve quality of life—to patients facing life-limiting illnesses. She said findings from this study should force new discussions.
“These are conversations that need to be had,” she said. “This brings us to a new era of asking how to right-size care, and how to bring evidence to that issue. There is an important message here that taking things away isn’t always bad.”
###
In addition to Abernethy, study authors include Don Taylor at Duke, along with Jean Kutner, Diane Fairclough and Patrick J. Blatchford at the University of Colorado; Laura Hanson at the University of North Carolina; Christine Ritchie at the University of California, San Francisco; and Janet Bull, Four Seasons.
The National Institute of Nursing Research provided funding for the study (UC4-NR012584, U24-NR014637).
###
Sarah Avery
[email protected]
919-660-1306
Duke University Medical Center
Scientists discover potential new target for cancer immunotherapy

|
Scientists have found a way to target elusive cells that suppress immune response, depleting them with peptides that spare other important cells and shrink tumors in preclinical experiments, according to a paper published online by Nature Medicine.
“We’ve known about these cells blocking immune response for a decade, but haven’t been able to shut them down for lack of an identified target,” said the paper’s senior author, Larry Kwak, M.D., Ph.D., chair of Lymphoma/Myeloma and director of the Center for Cancer Immunology Research at The University of Texas MD Anderson Cancer Center.
The cells, called myeloid-derived suppressor cells (MDSCs), are found abundantly in the microenvironment around tumors. Created with other blood cells in the bone marrow, they interfere with activation and proliferation of T cells, the immune system’s attack cells. MDSCs have been shown in mouse models to accelerate cancer progression and metastasis.
“This is the first demonstration of a molecule on these cells that allows us to make an antibody, in this case a peptide, to bind to them and get rid of them,” Kwak said. “It’s a brand new immunotherapy target.”
Kwak has developed anti-cancer therapeutic vaccines to spark an immune system attack against tumors, but their effectiveness has been hindered by factors such as MDSCs that stifle immune response. “The key to taking cancer vaccines to another level is combining them with immunotherapies that target the tumor microenvironment,” Kwak said.
Antibodies only bind to target cells
Peptide antibodies developed by Kwak and co-discoverer, Hong Qin, Ph.D., assistant professor of Lymphoma/Myeloma, wipe out MDSCs in the blood, spleen and tumor cells of mice without binding to other white blood cells or dendritic cells involved in immune response.
What is Immunotherapy?
This section has been reviewed and approved by the Cancer.Net Editorial Board, 3/2013
Immunotherapy (also called biologic therapy or biotherapy) is a type of cancer treatment designed to boost the body’s natural defenses to fight the cancer. It uses materials either made by the body or in a laboratory to improve, target, or restore immune system function. Although it is not entirely clear how immunotherapy treats cancer, it may work by stopping or slowing the growth of cancer cells, stopping cancer from spreading to other parts of the body, or helping the immune system increase its effectiveness at eliminating cancer cells.
There are several types of immunotherapy, including monoclonal antibodies, non-specific immunotherapies, and cancer vaccines.
Monoclonal antibodies
When the body’s immune system detects antigens (harmful substances, such as bacteria, viruses, fungi, or parasites), it produces antibodies (proteins that fight infection). Monoclonal antibodies are made in a laboratory, and when they are given to patients, they act like the antibodies the body produces naturally. Monoclonal antibodies are given intravenously (through a vein) and work by targeting specific proteins on the surface of cancer cells or cells that support the growth of cancer cells. When monoclonal antibodies attach to a cancer cell, they may accomplish the following goals:
Allow the immune system to destroy the cancer cell. The immune system doesn’t always recognize cancer cells as being harmful. To make it easier for the immune system to find and destroy cancer cells, a monoclonal antibody can mark or tag them by attaching to specific parts of cancer cells that are not found on healthy cells.
Prevent cancer cells from growing rapidly. Chemicals in the body called growth factors attach to receptors on the surface of cells and send signals that tell the cells to grow. Some cancer cells make extra copies of the growth factor receptor, which makes the cancer cells grow faster than normal cells. Monoclonal antibodies can block these receptors and prevent the growth signal from getting through.
Deliver radiation directly to cancer cells. This treatment, called radioimmunotherapy, uses monoclonal antibodies to deliver radiation directly to cancer cells. By attaching radioactive molecules to monoclonal antibodies in a laboratory, they can deliver low doses of radiation specifically to the tumor while leaving healthy cells alone. Examples of these radioactive molecules include ibritumomab tiuxetan (Zevalin) and tositumomab (Bexxar).
“That’s really exciting because it’s so specific for MDSCs that we would expect few, if any, side effects,” Kwak said. The team is working to develop the same target for use in humans.
With no candidate targets, the team took an objective approach by applying a peptide phage library to MDSCs, which permitted mass screening for candidate peptides - short sequences of amino acids - that bind to the surface of the MDSCs.
Peptide phage gathered from the MDSCs were expanded, enriched and then sequenced to identify predominant peptides. The team found two, labeled G3 and H6, that bound only to MDSCs; other candidates were eliminated because they also tied in to other types of cell.
They fused the two peptides to a portion of mouse immune globulin to generate experimental “peptibodies.” Both peptibodies bound to both types of MDSC - monocytic white blood cells, which engulf large foreign bodies or cell debris, and granulocytic white cells loaded with tiny granules.
The researchers treated mice with two types of thymus tumor with each peptibody, a control peptibody and an antibody against Gr-1. The G3 and H6 peptibodies depleted both types of MDSC in the blood and spleens of mice in both tumor models, while the Gr-1 antibody only worked against granulocytic MDSC.
Both peptibodies also wiped out the MDSCs in both types of thymic tumor and in the blood and spleen of mice with lymphoma.
Shrinking tumors, identifying alarmins
To see whether MDSC depletion would impede tumor growth, they treated mice with thymic tumors with the peptides every other day for two weeks. Mice treated with either pep-G3 or pep-H6 had tumors that were about half the size and weight of those in mice treated with controls or the Gr-1 antibody.
IMMUNOTHERAPY IS ONE OF THE MOST RECENT ADVANCES IN CANCER THERAPY
Radiation, chemotherapy, and surgery are the traditional tools in the fight against cancer. Radiation was discovered in the 1800’s by Marie Curie. Chemotherapy evolved from mustard gas (World War 1), and surgery dates back to the ancient Egyptians.
These treatment modalities are all based on destroying cancer cells by burning them (irradiation), poisoning them (chemotherapy) or removing them (surgery). While they can effectively kill or remove cancer cells, the use of these treatments often is limited because large numbers of healthy cells also tend to be destroyed. This often results in extreme morbidity and/or disfigurement of the patients treated with them. In the worst cases, these treatments can sometimes result in the patient’s death.
To date, there is no “magic bullet” in the treatment of cancer, and because of the complexity of cancer biology, it will likely not be attainable. It is now generally agreed that the future of cancer therapy lies in the combination of therapies with different mechanisms of action.
Immunotherapy is one of the more recent approaches to cancer therapy. It is based on the generally-accepted hypothesis that the immune system is the best tool humans have for fighting disease.
Immunotherapies have the potential to be used to fight cancer by either applying an external stimulus to the immune system to make it act more ‘forcefully’ or ‘smarter’, or by providing the immune system with man-made or naturally-derived tumor specific proteins made outside of the body so that the immune system can recognize the tumor as a foreign entity and destroy it.
Immunotherapy is sometimes used by itself to treat cancer, but it is most often used in combination with traditional treatments like radiation, chemotherapy, and surgery in order to enhance their effects. One of the possible benefits of immunotherapy is that it has the potential not to be as toxic as radiation, chemotherapy, and surgery. In addition, immunotherapy often may offer a different mode of attack on the tumor, thereby affording both patients and doctors alike a potential new treatment in the fight against cancer.
Analysis of surface proteins on the MDSCs identified S100A9 and S100A8 as the likely binding targets for the two peptibodies. They’re members of the S100 family of proteins, called alarmins, which are released outside the cell as a danger signal in response to inflammation.
MDSCs’ mechanisms for blocking immune response are not well-characterized because they’ve been hard to study for lack of a targeting method, Kwak said.
Kwak and colleagues are working to extend their findings to human MDSCs.
A new class of drugs called immune checkpoint inhibitors block molecules on T cells that shut down immune response, freeing the immune system to attack tumors. The first of these drugs, ipilimumab (Yervoy®) was approved by federal regulators to treat advanced melanoma. It’s the only drug ever to lengthen survival for those patients. Additional immune checkpoint inhibitors are under development.
“Immune checkpoint blockade is great,” Kwak said. “There have been dramatic response rates, but those drugs also have side effects. Targeting MDSCs could provide an additional way to unleash the immune system.”
###
Co-authors with Kwak and first author Qin are Beatrisa Lerman, Ippei Sakamaki, M.D., Ph.D., Guowei Wei, Ph.D., Soungchul Cha, Ph.D., Sheetal Rao, Jianfei Qian, Ph.D., and Qing Yi, M.D., Ph.D., all of Lymphoma/Melanoma; Yared Hailemichael, Ph.D., and Willem Overwijk, Ph.D., of Melanoma Medical Oncology; Roza Nurieva, Ph.D., of Immunology; and Karen Dwyer, Ph.D., and Johannes Roth, Ph.D., of Stem Cell Transplantation and Cellular Therapy; all are associated with the Center for Cancer Immunology Research.
Lerman is a graduate student in The University of Texas Graduate School of Biomedical Sciences, a joint program of MD Anderson and The University of Texas Health Science Center at Houston.
Funding for this research was provided by MD Anderson’s Specialized Program in Research Excellence in Lymphoma from the National Cancer Institute of the National Institutes of Health (P50 CA136411).
About MD Anderson
The University of Texas MD Anderson Cancer Center in Houston ranks as one of the world’s most respected centers focused on cancer patient care, research, education and prevention. MD Anderson is one of only 41 comprehensive cancer centers designated by the National Cancer Institute (NCI). For ten of the past 12 years, including 2013, MD Anderson has ranked No. 1 in cancer care in “Best Hospitals,” a survey published annually in U.S. News & World Report. MD Anderson receives a cancer center support grant from the NCI of the National Institutes of Health (P30 CA016672).
###
Scott Merville
[email protected]
713-516-4855
University of Texas M. D. Anderson Cancer Center
To curb hepatitis C, test and treat inmates

|
Problematic as it is for society, the high incarceration rate in the United States presents an important public health opportunity, according to a new “Perspective” article in the New England Journal of Medicine. It could make staving off the worst of the oncoming hepatitis C epidemic considerably easier.
Nearly 4 million Americans may be infected with the hepatitis C virus (HCV). Many of them don’t know they carry HCV, which can take decades to make them ill with cirrhosis, cancer, or liver failure. About a million people could die because of HCV by 2060, the authors wrote, and many who are saved will have required critical and costly treatments, including liver transplants.
“We know this is going to come crashing down on us,” said lead author Dr. Josiah D. Rich, professor of medicine and epidemiology at Brown University and director of the Center for Prisoner Health and Human Rights at The Miriam Hospital. “It’s already starting to come crashing down. The next 10 to 20 years are going to be ugly.”
The single best setting for fighting the epidemic is U.S. prisons and jails, where more than 10 million people cycle through each year. In part because a major means of HCV transmission is through injection drug use, a large portion of the nation’s infected population passes through the criminal justice system. In the journal, for example, Rich and his coauthors estimate that one in six inmates is infected and one in three infected Americans ends up locked up for at least a little time in their lives.
“We can head off a lot of disease and expense if we invest now,” Rich said. “How do we do that most efficiently and effectively? What we’re arguing in the paper is that we do it using the criminal justice system infrastructure.”
Worth the considerable cost
The key barrier, Rich readily acknowledges, is the very high cost of hepatitis C drugs. A 12-week course of Sovaldi, made by Gilead Sciences, costs $84,000 a person. Treating all current inmates with HCV would therefore cost $33 billion, the authors estimate. Treating just half the people who cycle through prisons and jails in a given year would cost $77 billion.
But drug costs don’t have to be nearly so high if state prison systems can negotiate reasonable discounts with drug makers, as the federal government does for its prisoners.
And while prisons have a clear disincentive to spend money to treat people who may well be released before they become sick, the money cannot and need not come solely from their budgets.
“The criminal justice system cannot be expected to shoulder the prohibitive costs of hepatitis C treatments alone,” said co-author Dr. Brie A. Williams, associate professor of Medicine at the University of California - San Francisco. “Recognizing that infectious disease epidemics cannot be contained behind prison walls, we must develop a national strategy for responding to them that includes financial support and an infrastructure to test and treat prisoners, both within prisons and jails and after they return to our communities.”
U.S. society as a whole will pay the costs of an inadequately addressed HCV epidemic, the authors said. Helping prisons to provide this treatment will also curb the need for litigation by prisoner advocates to a community standard of HCV care for prisoners, said co-author Dr. Scott A. Allen, professor of medicine at the University of California - Riverside.
“Even with the high cost, the drugs appear to be cost-effective,” Allen said. “Private insurers in the community appear to be covering it. That establishes a clear community standard, and prisons will be held to that standard by the courts. The public policy question isn’t whether or not we pay for hepatitis C care but how we pay for it.”
A potential model already exists in the Ryan White Care Act, the three authors note. Congress could consider replicating that achievement of funding widespread HIV services and treatment for people who couldn’t obtain them otherwise them. An HCV version could include programs and grants for prisons and jails, as well as programs to prevent reinfection of inmates after they are released.
“Seizing this opportunity for timely care will require leaders to consider the criminal justice system as part of the fabric of U.S. health care,” the authors concluded. “This step will help to change the perception of the HCV epidemic in the criminal justice system, transforming it from a legal liability to a critical opportunity to change the course of HCV in the United States.”
###
The research for the article required no direct funding, but Rich disclosed an honorarium he received from Gilead for speaking at a meeting in 2012.
###
David Orenstein
[email protected]
401-863-1862
Brown University
Study finds hazardous flame retardants in preschools

|
A new study of preschools and day care centers finds that flame retardants are prevalent indoors, potentially exposing young children to chemicals known to be hazardous.
The study, to appear online Thursday, May 15, in the journal Chemosphere, was led by researchers at the University of California, Berkeley, and funded by the California Air Resources Board. Although many infants and young children spend up to 50 hours per week in day care, the study authors noted that this paper represents the first systematic review of flame retardants in early child care settings.
The researchers covered 40 child care centers serving 1,764 children in Monterey and Alameda counties. The facilities were located in a mix of urban, rural and agricultural areas. The researchers collected air and floor dust samples when the children were present, and tested for 14 different PBDEs, or polybrominated diphenyl ethers, and four non-PBDE flame retardants, including tris phosphate compounds.
The study found both PBDEs and tris phosphate compounds in 100 percent of the dust samples collected. Median levels of PBDEs were somewhat lower than those found in homes in other studies, but median levels of chlorinated tris were similar to or higher than household levels found in other studies.
“These findings underscore how widespread these materials are in indoor environments,” said study lead author Asa Bradman, associate director of the Center for Children’s Environmental Health Research at UC Berkeley. “A growing body of research has found links between flame retardants and a range of human health effects, including neurodevelopmental delays in children. Children are more vulnerable to the health effects of environmental contaminants, so we should be particularly careful to reduce their exposure to harmful chemicals.”
While flame retardants were commonplace in dust, the good news is that levels of the chemicals were generally low in air samples.
Old flame retardant resurfaces
Of the facilities surveyed, 29 had upholstered furniture and 17 had napping equipment made out of foam. Facilities with foam had significantly higher concentrations of flame retardant chemicals than the centers without such equipment.
In response to growing health concerns about these chemicals, California banned the use of two types of PBDEs in 2006. Furniture manufacturers also began phasing them out, but products made before the ban are still found in many buildings.
The detection of the older class of flame retardants was more surprising. In the 1970s, UC Berkeley research by Arlene Blum, a postdoctoral researcher at the time, and Bruce Ames, UC Berkeley professor of molecular and cell biology, showed that brominated tris was a mutagen and presumed carcinogen. That work helped lead to the chemical’s removal from children’s sleepwear.
“I remember learning about the tris phosphate flame retardants in kids’ pajamas when I was in high school 35 years ago, so it’s a bit surprising to still be seeing them today,” said Bradman. “They were never banned. There seems to have been a resurgence in recent years as manufacturers looked for PBDE replacements.”
Earlier this year, the California Department of Toxic Substances Control identified children’s foam sleeping pads containing flame retardants as one of three products considered harmful to consumers. Agency officials specifically cited nap mats, bassinets and infant travel beds as items that commonly contain chlorinated tris phosphate, a carcinogen and hormone-disrupter.
Change in flammability standards could mean fewer chemicals
New changes in state flammability standards may soon eliminate the need to use those chemical replacements. Previous regulations required the foam in consumer items to withstand a small open flame for 12 seconds without igniting.
Blum, now executive director of the Green Science Policy Institute and a UC Berkeley visiting scholar in chemistry, noted that the old standard, known as TB117, did not help fire safety since it is the fabric covering the foam that needs to be fire resistant. The standard, she noted, had led to the extensive use of flame retardants in furniture and foam baby products without providing a fire safety benefit.
Gov. Jerry Brown, presented with evidence that the flame retardant chemicals are linked to health concerns, ordered an update to the state flammability standard. The new regulation, TB117-2013, requires fabrics of upholstered furniture to withstand smolders, such as from lit cigarettes. It takes effect this year, and will be mandatory by January 2015.
“The new standard is not a ban on flame retardants, but manufacturers can meet it without using the chemicals,” said Blum. “Most upholstered fabrics, such as leather, are already smolder-proof. Consumers should verify that the furniture they are buying is free of flame retardants, especially when children will be exposed.”
###
Other co-authors of the study include researchers from the Battelle Memorial Institute in Ohio, the U.S. Environmental Protection Agency, the Lawrence Berkeley National Laboratory and the California Air Resources Board.
###
Sarah Yang
[email protected]
510-643-7741
University of California - Berkeley
Access to electronic health records may influence care

|
Unlike medical records kept in paper charts, electronic health records (EHR) provide numerous access points to clinicians to review a patient’s medical history. A new study has found access to electronic health records in acute care situations may influence the care given to that patient, and in some cases, failure to review the EHR could have adversely affected the medical management. The findings are reported in the May 2014 edition http://content.healthaffairs.org/content/33/5/800.abstract of Health Affairs. John L. Ulmer, M.D., professor of radiology and chief of neuroradiology at the Medical College of Wisconsin (MCW), is the corresponding author. Co-authors are Michael J. Franczak and Madeline Klein, former research assistants at MCW; Flavius Raslau, M.D., assistant professor of radiology at the University of Kentucky College of Medicine; Jo Bergholte, program manager at MCW; and Leighton P. Mark, professor of radiology at MCW.
In the study, three neuroradiologists at Froedtert & the Medical College Froedtert Hospital analyzed 2,000 head CT scans that had been ordered by emergency department physicians. For each exam, the neuroradiologists compared the medical information generated by the emergency department physicians to the additional information retrieved by interpreting radiologists who had access to EHR patient data.
The interpreting radiologists found that in many of the cases, the additional data in the EHR would have a significant impact on the interpretations of the head CT scans.
In nine percent of the cases, the neuroradiologists predicted the interpretation would have “very likely” been adversely affected had the EHR data not been available. In 22 percent of cases, the additional clinical information found in the EHR was rated as “possibly” having a clinically significant impact on the interpretation of the head CT. “This study exemplifies the power of EHR’s and their potential impact on patient care and positive outcomes. Health care providers must recognize the value of implementing EHR’s and foster their widespread adoption,” said Dr. Ulmer. “The federal government has made a significant investment in the adoption of these systems, particularly with the challenges of expanding remote access to high-quality care.”
###
Maureen Mack
[email protected]
414-955-4744
Medical College of Wisconsin
Cholesterol drug users may use pills as a license to overeat

|
People who take the common cholesterol-lowering drugs known as statins may feel a false sense of security and eat a bit more, according to a new study.
Researchers found that U.S. adults taking statins in 1999-2000 were eating fewer calories than people not taking the drugs, but statin users were eating about the same amount as non-users by 2009-2010.
“We believe that physicians need to reemphasize the importance of a healthy lifestyle to statin-users,” Dr. Takehiro Sugiyama told Reuters Health in an email.
He is the study’s lead author from the University of Tokyo in Japan.
Eating excess calories and fat would not only compromise the cholesterol-lowering effect of statins, he said. It would also increase a person’s risk of becoming obese and developing diabetes.
Statins - such as Lipitor, Zocor and Crestor - inhibit the production of cholesterol, which is used to build new cells and keep the body functioning. Too much cholesterol increases a person’s chances of developing heart disease and fatty deposits in blood vessels, however.
Under new recommendations from the American College of Cardiology and the American Heart Association, the number of U.S. adults eligible to take the drugs may reach 56 million.
The new guidelines deemphasize the use of LDL or “bad” cholesterol as a measure of when to put people on the drugs. Instead, doctors are encouraged to take several risk factors into account to target people at high risk for heart attacks or strokes (see Reuters story of November 12, 2013 here: reut.rs/QFucA3.)
Previous studies had found no evidence that statin users eat more after being prescribed the drugs, the authors write in JAMA Internal Medicine. Use of the drugs has increased substantially since those studies were conducted, however.
For the new study, the researchers used data from a national survey of U.S. adults that’s conducted every two years.
They found that statin users were consuming about 2,000 calories per day in 1999-2000, on average, compared to about 2,179 calories per day among non-users.
Sugiyama writes that it would be expected that stain users eat less in an attempt to control their cholesterol and weight.
Calorie consumption among the statin users increased as time went on, however. By 2005-2006 there were no differences between the two groups.
Overall, calorie consumption among statin users increased by about 10 percent during the decade. Statin users significantly increased the amount of calories they got from fat during the study period, too.
Meanwhile, calorie and fat consumption remained unchanged among people not taking statins.
Sugiyama said there could be two explanations for the findings.
“We suppose (patients) noticed the potency of the statin treatment because their LDL-cholesterol level would drop drastically regardless of no change on diet,” he said. “Through this process, statin users may learn that they do not need to restrict their diet to achieve the LDL-level goal.”
Alternatively, doctors may have started prescribing statins to people who tend to eat more and they may not be as reluctant to prescribe the drugs to people who don’t control their diets.
“Because of the study design, we were not able to disentangle the mechanism,” he said.
The research also can’t say for certain that statins caused people to eat more as time went on. There could be another unknown factor that influenced the results.
“I think the biggest impact of this trial is that as physicians when we put patients on statins it shouldn’t be the end of the discussion about other lifestyle interventions,” Dr. David Frid said.
Frid is a staff cardiologist at the Cleveland Clinic in Ohio. He was not involved with the new study.
“Even on a statin, you do need to continue following your dietary recommendations,” he told Reuters Health.
Sugiyama agreed that statin use should be paired with lifestyle modification.
“Over-relying on medication would cause side effects, unnecessary medical costs and perhaps an ethical concern,” he said. “I think physicians need to reemphasize the importance of dietary control for statin-users.”
SOURCE: JAMA Internal Medicine, online April 24, 2014.
Study ties breathing problems, asthma to bone loss

|
People with asthma-related breathing problems may be at increased risk for bone loss, according to a new study.
The study examined the records of more than 7,000 adults in Seoul, Korea, and found those with a certain characteristic of asthma had significantly lower bone density in a region of their spine than those without asthma symptoms.
The characteristic, called airway hyperresponsiveness, means the airways in the lungs are particularly sensitive, and it doesn’t take much to trigger an asthma attack.
However, both men and women with airway hyperresponsiveness were still in the normal range for overall bone density, on average. And researchers couldn’t say whether the asthma symptoms or the bone loss came first or what linked the two.
“Asthma could be a risk for bone loss. The degree to which their disease puts them at risk for bone loss and fractures needs to be further studied,” Dr. Sonal Singh told Reuters Health.
“We should be thinking about fractures in patients with asthma,” he said. “The study did make me think about the link between asthma and bone loss as I see my patients.”
Singh, from Johns Hopkins University School of Medicine in Baltimore, Maryland, was not involved in the current research but has studied broken bones in people taking steroids for chronic obstructive lung disease.
 The Centers for Disease Control and Prevention estimates that 25 million Americans - or one in 12 - have asthma. The U.S. Surgeon General in 2012 predicted that by 2020 half of Americans over age 50 could have weak bones.
The Centers for Disease Control and Prevention estimates that 25 million Americans - or one in 12 - have asthma. The U.S. Surgeon General in 2012 predicted that by 2020 half of Americans over age 50 could have weak bones.
For the new study, researchers led by Dr. Jae-Woo Jung of Seoul National University Medical Research Center analyzed the health records of 7,034 patients seen at their hospital.
They found average bone density was lower in the lumbar spine in the 216 people who tested positive for airway hyperresponsiveness.
The lumbar spine is the region between the ribs and the pelvis.
In addition, about 45 percent of those patients had osteopenia, or lower than normal bone density, and six percent had osteoporosis. That compared to a 30 percent rate of osteopenia and a four percent rate of osteoporosis among people without airway hyperresponsiveness, according to findings published in the Annals of Allergy, Asthma & Immunology.
 The study also found a lower bone density in the lumbar spines of people who reported having been diagnosed with asthma than in people without asthma. But Singh said it was hard to know whether that was meaningful, because the researchers didn’t measure asthma objectively.
The study also found a lower bone density in the lumbar spines of people who reported having been diagnosed with asthma than in people without asthma. But Singh said it was hard to know whether that was meaningful, because the researchers didn’t measure asthma objectively.
Previous studies have found lower vitamin D levels among patients with asthma and related symptoms, the authors write.
They did not respond to a request for comment but speculate in the study that vitamin D deficiency might factor into bone loss among people with asthma and airway hyperresponsiveness.
The current study did not measure participants’ vitamin D levels, so it can’t say anything about the vitamin’s link to asthma and bone loss.
Fractures are a known side effect of the systemic steroids used to treat asthma, Jung and colleagues write. Several studies have also tied inhaled steroids to decreased bone density, they note.
Steroids can decrease bone formation by stopping calcium from being absorbed. The drugs can also interfere with production of sex hormones, causing muscle weakness and raising the risk of falls and related fractures, according to the National Institutes of Health.
The NIH also says that people with asthma may avoid calcium-rich milk and other dairy products as well as weight-bearing exercise - key ingredients for bone health.
In the new study, the researchers excluded patients who had used systemic steroid medications. But the study did not consider participants’ use of inhaled steroids or other drugs for control of asthma and related symptoms.
Singh said the study prompted him to want to examine asthma and bone loss in research considering ethnicity, physical activity, vitamin D levels and use of inhaled steroids.
SOURCE: Annals of Allergy, Asthma & Immunology, online March 20, 2014
Arkansas to appeal ruling on abortion restriction law

|
Arkansas Attorney General Dustin McDaniel said on Friday he would appeal a federal judge’s decision striking down a state law that bans most abortions starting at 12 weeks of pregnancy, one of the most stringent such statutes in the United States.
U.S. District Judge Susan Webber Wright ruled last month that the Arkansas law violated the U.S. Supreme Court decision that a woman has the right to an abortion until the fetus is viable outside the womb, which medical experts say is around the 23-to-24-week mark
A number of states have recently enacted restrictive bans on abortion, including North Dakota, Arizona and Texas, setting off a round of court battles.
Arkansas Governor Mike Beebe, a Democrat, vetoed the law after it was passed by the Republican-controlled state legislature in March 2013, citing its conflict with Supreme Court doctrine, but his veto was overridden.
McDaniel, who had previously echoed Beebe’s reservations about the bill, said in a statement he would appeal the ruling with the 8th U.S. Circuit Court of Appeals, in St. Louis.
As enacted, the Arkansas Human Heartbeat Protection Act would have banned most abortions at or after 12 weeks of pregnancy, if a fetal heartbeat could be detected by standard ultrasound.
Doctors who were found to violate the statute would have risked having their licenses revoked by the state medical board.
Exemptions would have been allowed in cases where the pregnancy resulted from rape or incest, if the life of the mother was in danger, or in cases of a gross fetal abnormality that made the fetus’ survival impossible.
(Editing by Paul Thomasch and Leslie Adler)
###
By Lisa Bose McDermott
Supreme Court declines to hear new contraception cases

|
The U.S. Supreme Court on Monday declined to take up preliminary appeals brought by Roman Catholic groups that want an exemption from part of President Barack Obama’s healthcare law requiring employers to provide insurance that covers contraception.
The cases were brought by a series of Roman Catholic-affiliated nonprofit groups based in Washington, D.C., including Catholic University.
The legal issue is different from one involving for-profit companies that also object on religious grounds to the so-called contraception mandate, which was argued before the high court last week.
The Supreme Court’s decision not to hear the two cases at this stage means that the federal appeals court in Washington will proceed to decide the issue. If the groups lose, they would have another chance to seek Supreme Court review.
The Obamacare law requires employers to provide health insurance policies that cover preventive services for women, including contraception and sterilization. The act makes an exception for religious institutions such as houses of worship that mainly serve and employ members of their own faith, but not for schools, hospitals and charitable organizations that employ people of all faiths.
As a compromise, the administration agreed to an accommodation for non-profits affiliated with religious entities that was finalized in July 2013. But the various Catholic groups said the compromise process still violated their religious rights, prompting a new wave of litigation.
Courts across the country have granted the groups injunctions which prevent the administration from enforcing the mandate during the litigation.
The cases are Roman Catholic Archbishop of Washington v. Sebelius and Priests for Life v. U.S., U.S. Supreme Court, 13-891 and 13-829.
(Reporting by Lawrence Hurley; Editing by Howard Goller and James Dalgleish)
###
(Reuters)
Tamiflu-resistant influenza: Parsing the genome for the culprits
.jpg)
|
Tamiflu is one of the few available treatments for those who come down with the flu. But the virus quickly develops resistance; multiplying at a rate of several generations a day, these tiny pathogens rapidly accumulate genetic mutations. Because of this, they have a good chance of developing counterattacks to the antiviral. How can these infinitesimal variations be identified within the immensity of the virus’ genetic code? EPFL researchers have created a computer tool that can shed light on the flu virus’ formidable adaptability. They were able to find mutations that conferred resistance that had up to this point not yet been identified. Their software has been made freely available to researchers everywhere, and is the subject of an article published in the journal PLOS Genetics.
Widespread use of Tamiflu leads to resistance
In theory, Tamiflu should only be used by patients in fragile health. But during the 2008-2009 flu season, the drug was used for the first time on a very wide scale. Resistant strains of the virus appeared within just a few weeks. Fortunately, even though the mutation induced a resistance to Tamiflu, it also caused a reduction in the replication rate of the virus. Once the use of the antiviral was dialed back to a more reasonable level, the resistant strains lost their competitive advantage, and they disappeared, submerged by competitors that were sensitive to the drug but had a higher rate of replication.
Resistance always results from random mutations, says Jeffrey Jensen, co-author of the EPFL study. But when a mutation leads to a competitive advantage, for example the ability to resist against a source of aggression, it tends to be passed on to its descendants. “A priori, nothing distinguishes one mutation from another; they’re all the result of chance. Our goal is precisely to be able to tell the difference between mutations that make the virus resistant to Tamiflu, thus leading to a selection phenomenon, and other mutations.”
New resistant mutations are discovered
To begin, the team led by Jensen and his colleague Matthieu Foll cultured ordinary H1N1 virus in the laboratory. Certain groups were subjected to Tamiflu, others not. Every 48 hours - 13 generations - the biologists sequenced the virus’ genome to reveal the genetic mutations that had occurred in the interval.
The more the genetic mutations of viruses exposed to Tamiflu tended to become prevalent with time, the higher the probability that they would confer resistance. With a complex statistics-based software tool, the researchers were able to pinpoint 12 sites on the viral genome that carried suspect variations. One of these was already known, but the rest had not yet been identified.
Weeding out the resistance-conferring mutations
Using their statistical software, the researchers were able to comb through the immensity of the viral genetic code and identify only the mutations that were suspected to cause resistance, with a certainty of more than 99% - making their software a powerful tool indeed.
And these newly discovered mutations are reason for concern: they could allow the virus to be resistant while maintaining an elevated reproductive capacity. Jensen thus doesn’t exclude the possibility that pathogenic strains could appear that are both competitive and Tamiflu-resistant, if the mistake of 2008-2009 is repeated. For Foll, first author on the study, “the risk is real, and we need to investigate further.”
###
Lionel Pousaz
[email protected]
41-795-597-161
Ecole Polytechnique Fédérale de Lausanne
Optimism linked to healthier eating among women

|
Women with a sunny disposition may also have an easier time adopting healthy habits, according to a new study.
Researchers found that women who were more optimistic were better able to follow healthy eating guidelines, both when they were instructed to do so and when they chose to make changes on their own.
The authors noted that the biggest help for making diet improvements is not necessarily optimism itself, but the skills that tend to go with it.
“It’s not just having a sunny outlook - rather, this is a marker of other things people do,” said Melanie Hingle, a dietician at the University of Arizona in Tucson. She led the new study, which was published in the Journal of the Academy of Nutrition and Dietetics.
“People who want to make lifestyle changes should focus on skill-based factors that can help them whether or not they are an optimist,” she told Reuters Health.
The study used data collected as part of the Women’s Health Initiative, a study of a national sample of postmenopausal women between the ages of 50 and 79.
The researchers analyzed data from two groups of women: more than 13,500 who had been part of a program to improve their nutrition - mainly by decreasing fat intake - and another 20,000-plus who were not asked to make any changes to their diet.
The women’s optimism levels had been evaluated with a questionnaire as part of the study. Another survey aimed to evaluate the overall healthfulness of participants’ diets at the beginning of the study and one year later.
Hingle and her team found that the most optimistic one third of the women saw the most improvement in their diets, whether or not they had completed the nutrition program.
On a scale measured from zero to 110, where higher numbers indicate better diet quality, women with the highest optimism in the nutrition program improved their diet by 1.8 points, and those with the lowest optimism improved their diet by 1.4 points. Among women not in the program, scores improved by 1.0 point for those with the highest initial optimism and by 0.3 points for those with the lowest. The differences were considered statistically meaningful.
The least optimistic women also started out with less-healthy diets, on average, than those who had sunnier dispositions.
Yet optimism itself is almost beside the point, Hingle said.
People who want to adopt healthier behaviors - whether quitting smoking, eating more vegetables or getting more exercise - should instead focus on the skills that tend to make optimistic people successful at those ventures, she said.
“You can’t tell someone who’s a pessimist to be an optimist. Instead, look at the traits that make optimists successful,” Hingle said.
One such skill is self-regulation, or being aware of one’s behavior as it is unfolding. In the case of healthy eating, that includes monitoring eating habits, whether by making a mental note or keeping tabs in a journal.
Self-regulation is “choosing what you are eating and making a conscious decision in that moment,” Hingle said.
Another strategy to successfully adopt a new habit is finding healthy ways to cope with unpleasant emotions and stress instead of, for example, eating junk food or smoking. For junk food addicts, that means getting the unhealthy foods they tend to reach for when stressed - whether potato chips, cake or sugary soft drinks - out of the house, and channeling frustration into something more productive.
“It’s about finding a different activity to occupy that moment when you’re feeling stressed, such as coping with breathing exercises, talking to a friend, going for a walk or even going through some guided imagery,” Hingle said.
“The goal is to help you move past that stressful moment instead of reaching for food,” she said.
Optimistic people may also have better social support, whether as a cause or a result of their more-positive thinking. That’s important because the support of friends and family can make it easier to get healthy.
The point, Hingle said, is that learning new skills can help anyone trying to turn over a new leaf.
“It doesn’t really matter if you’re an optimist or a pessimist. Either way, you can make positive changes to your diet,” she said.
SOURCE: Journal of the Academy of Nutrition and Dietetics, online February 21, 2014.
###
Optimism and Diet Quality in the Women’s Health Initiative
Diet quality has not been well studied in relation to positive psychological traits. Our purpose was to investigate the relationship between optimism and diet quality in postmenopausal women enrolled in the Women’s Health Initiative observational study (OS) and clinical trials (CTs), and to determine whether optimism was associated with diet change after a 1-year dietary intervention. Diet quality was scored with the Alternate Healthy Eating Index (AHEI) and optimism assessed with the Life Orientation Test-Revised. Baseline characteristics were compared across AHEI quintiles or optimism tertiles using regression models with each variable of interest as a function of quintiles or tertiles (OS, n=87,630; CT, n=65,360). Association between optimism and baseline AHEI and change in AHEI over 1 year were tested using multivariate linear regression (CT, n=13,645). Potential interaction between optimism and trial arm and demographic/lifestyle factors on AHEI change was tested using likelihood ratio test (CT intervention, n=13,645; CT control, n=20,242). Women reporting high AHEI were non-Hispanic white, educated, physically active, past or never smokers, hormone therapy users, had lower body mass index and waist circumference, and were less likely to have chronic conditions. In the CT intervention, higher optimism was associated with higher AHEI at baseline and with greater change over 1 year (P=0.001). Effect modification by intervention status was observed (P=0.014), whereas control participants with highest optimism achieved threefold greater AHEI increase compared with those with the lowest optimism. These data support a relationship between optimism and dietary quality score in postmenopausal women at baseline and over 1 year.
Melanie D. Hingle, Betsy C. Wertheim, Hilary A. Tindle, Lesley Tinker, Rebecca A. Seguin, Milagros C. Rosal, Cynthia A. Thomson
Journal of the Academy of Nutrition and Dietetics - 21 February 2014 (10.1016/j.jand.2013.12.018)
U.S. advisers back DNA-based colon cancer test

|
A colon cancer screening method that analyzes DNA from stool samples won the unanimous backing of a U.S. advisory panel on Thursday, paving the way for potential regulatory approval of the non-invasive test.
A panel of outside experts advising the Food and Drug Administration voted 10-0 to recommend approval of the Cologuard screening test made by Exact Sciences Corp.
The company said a large clinical trial found that its test detected 92.3 percent of colorectal cancers in average-risk patients based on a combination of DNA and hemoglobin markers.
While a colonoscopy is considered the most accurate method of detecting colon cancer and polyps, many people avoid the test, which involves inserting a flexible tube into the colon.
If Cologuard is approved by the FDA, patients who have a positive cancer finding with the test, which identifies abnormal cells shed in the stool, would then undergo a colonoscopy.
The FDA usually follows panel recommendations, although it is not required to.
The American Cancer Society estimates about 50,000 deaths from colorectal cancer in the United States this year. It is the third leading cause of cancer-related deaths in the United States when men and women are considered separately, and the second leading cause when both sexes are combined.
Shares of Exact Sciences, which were halted on the Nasdaq on Thursday, were up 75 cents, or 5.5 percent at $14.50 in after-hours trading. The shares have gained more than 40 percent over the past 12 months.
###
(Reuters)
Pfizer lung cancer drug beats chemo for previously untreated patients

|
Pfizer Inc’s Xalkori delayed progression of lung cancer longer than chemotherapy in patients who had never previously been treated for the disease, according to results of a late-stage study released on Tuesday.
The medicine, which received U.S. approval in 2011 for lung cancer patients who have a specific gene mutation, had shown in a previous Phase III trial that it significantly delayed disease progression among those who have already undergone chemotherapy for non-small-cell lung cancer, the most common form of the illness.
Pfizer said favorable results from the latest trial, combined with those from the earlier big study, establish that Xalkori is appropriate for first-line as well as second-line use, meaning for patients receiving initial treatment as well as for those who have already undergone chemotherapy.
The drug is used among patients who have a mutation in the so-called ALK gene, as determined by an approved diagnostic test. The mutation only occurs in a small percentage of patients with lung cancer, but makes them good candidates for treatment with Xalkori.
Xalkori, with current annual sales of about $350 million, is expected to get a significant boost from the new data. Cowen and Co has predicted the medicine will generate annual peak sales of $1.05 billion by 2020.
Pfizer is also developing an array of other cancer medicines that work through new mechanisms, with the aim of becoming a major player in the oncology field.
Pfizer shares were up 0.6 percent at $31.67 in midday trading on the New York Stock Exchange.
(Reporting by Ransdell Pierson; Editing by Lisa Von Ahn and Andrew Hay)
###
(Reuters)
Mass. General study identifies path to safer drugs for heart disease, cancer

|
Massachusetts General Hospital (MGH) investigators may have found a way to solve a problem that has plagued a group of drugs called ligand-mimicking integrin inhibitors, which have the potential to treat conditions ranging from heart attacks to cancer metastasis. In a Nature Structural & Molecular Biology paper receiving advance online publication, the researchers provide a structural basis for the design of new and safer integrin inhibitors.
Integrins are receptor proteins found on the surface of cells that determine whether or not cells adhere to adjacent cells and the surrounding extracellular matrix. Under normal circumstances, integrins only become activated - which allows them to bind to other cells or extracellular molecules - in response to specific signals from within the cell. If integrins become overactive, cells become too “sticky” - leading to clogged arteries, pathological inflammation, the excess tissue growth called fibrosis or the spread of cancer. Current drugs developed to inhibit integrin activation by mimicking the shape of ligands - the molecules that interact with receptors - have had unintended effects in some patients, and as a result only a handful have received FDA approval.
“Integrins have an intrinsic ability to shape-shift when they switch from an inactive to an active, adhesive state,” explains M. Amin Arnaout, MD, director of the MGH Leukocyte Biology Program and the Inflammation and Structural Biology Program, senior author of the study. “Unfortunately, under some circumstances the integrin inhibitors that have been developed to date can inadventently induce this shape shifting, and use of these drugs have produced serious, sometimes fatal side effects such as excessive bleeding.”
In their search for drugs that would not induce these complications, the MGH team focused on an extracellular matrix protein called fibronectin, which binds to an integrin called αvβ3. Their detailed structural analysis of the bond between αvβ3 and various forms of FN10, the fibronectin molecule that interacts with αvβ3, identified a high-affinity version of FN10 that binds more strongly than the common form without causing unintended receptor activation. This first report of the three-dimensional atomic structure of an integrin binding with a ligand-mimicking molecule that does not cause inadvertent activation could enable the design of a new generation of integrin inhibitors without the complications that have limited their application.
###
The co-lead authors of the Nature Structural & Molecular Biology paper are Johannes van Agthoven, PhD, and Jain-Ping Xiong, PhD, of the Structural Biology Program in the MGH Department of Medicine. Additional co-authors are Brian Adair, PhD, Structural Biology Program; José Luis Alonso PhD, and Xianliang Rui, PhD, Leukocyte Biology and Inflammation Program, MGH Medicine; and Simon Goodman, DPhil, Merck KGaA, Germany. Arnaout is a physician and chief emeritus of the Division of Nephrology in the MGH Department of Medicine and a professor of Medicine at Harvard Medical School. The study was supported by National Institute of Diabetes and Digestive and Kidney Diseases grants DK088327, DK096334 and DK007540.
Massachusetts General Hospital, founded in 1811, is the original and largest teaching hospital of Harvard Medical School. The MGH conducts the largest hospital-based research program in the United States, with an annual research budget of more than $775 million and major research centers in AIDS, cardiovascular research, cancer, computational and integrative biology, cutaneous biology, human genetics, medical imaging, neurodegenerative disorders, regenerative medicine, reproductive biology, systems biology, transplantation biology and photomedicine.
###
Sue McGreevey
[email protected]
617-724-2764
Massachusetts General Hospital
Gates Foundation awards Notre Dame $23 million for malaria, dengue studies

|
The Bill & Melinda Gates Foundation has awarded $23 million for research being led by University of Notre Dame biologists to prevent malaria and dengue fever, the school said.
The five-year project by biologists Neil Lobo and Nicole Achee aims to show the effectiveness of a new method of mosquito control, called spatial repellency, in quelling the illnesses, the university said in a statement this week.
According to the World Health Organization, 207 million cases of malaria were reported in 2012, and 50 million to 100 million dengue infections occur yearly.
Both the malaria parasite and dengue virus are transmitted through the bites of infected mosquitoes. Spatial repellents, such as coils or candles, release a material that drives mosquitoes away from enclosed areas.
The Gates award is the second-largest to a single grant proposal at Notre Dame. A Microelectronics Advanced Research Corp award to fund the Center for Low Energy Systems Technology totaled $29 million.
(Reporting by Ian Simpson; Editing by Scott Malone and Lisa Von Ahn)
###
(Reuters)
More dangerous chemicals in everyday life: Now experts warn against nanosilver

|
Endocrine disrupters are not the only worrying chemicals that ordinary consumers are exposed to in everyday life. Also nanoparticles of silver, found in e.g. dietary supplements, cosmetics and food packaging, now worry scientists. A new study from the University of Southern Denmark shows that nano-silver can penetrate our cells and cause damage.
Silver has an antibacterial effect and therefore the food and cosmetic industry often coat their products with silver nanoparticles. Nano-silver can be found in e.g. drinking bottles, cosmetics, band aids, toothbrushes, running socks, refrigerators, washing machines and food packagings.
“Silver as a metal does not pose any danger, but when you break it down to nano-sizes, the particles become small enough to penetrate a cell wall. If nano-silver enters a human cell, it can cause changes in the cell”, explain Associate Professor Frank Kjeldsen and PhD Thiago Verano-Braga, Department of Biochemistry and Molecular Biology at the University of Southern Denmark.
Together with their research colleagues they have just published the results of a study of such cell damages in the journal ACS Nano.
The researchers examined human intestinal cells, as they consider these to be most likely to come into contact with nano-silver, ingested with food.
“We can confirm that nano-silver leads to the formation of harmful, so called free radicals in cells. We can also see that there are changes in the form and amount of proteins. This worries us”, say Frank Kjeldsen and Thiago Verano-Braga.
A large number of serious diseases are characterized by the fact that there is an overproduction of free radicals in cells. This applies to cancer and neurological diseases such as Alzheimer’s and Parkinson’s.
Kjeldsen and Verano-Braga emphasizes that their research is conducted on human cells in a laboratory, not based on living people. They also point out that they do not know how large a dose of nano-silver, a person must be exposed to for the emergence of cellular changes.
“We don’t know how much is needed, so we cannot conclude that nano-silver can make you sick. But we can say that we must be very cautious and worried when we see an overproduction of free radicals in human cells”, they say.
Nano-silver is also sold as a dietary supplement, promising to have an antibacterial, anti-flu and cancer-inhibatory effect. The nano-silver should also help against low blood counts and bad skin. In the EU, the marketing of dietary supplements and foods with claims to have medical effects is not allowed. But the nano-silver is easy to find and buy online.
In the wake of the Uiversity of Southern Denmark-research, the Danish Veterinary and Food Administration now warns against taking dietary supplements with nano-silver.
“The recent research strongly suggests that it can be dangerous”, says Søren Langkilde from the Danish Veterinary and Food Administration to the Danish Broadcasting Corporation (DR).
###
Ref: Insights into the Cellular Response Triggered by Silver Nanoparticles using Quantitative Proteomics. ACS NANO. http://dx.doi.org/10.1021/nn4050744
Photos of Frank Kjeldsen and Thiago Verano-Braga: SDU.
Contact
Associate Professor Frank Kjeldsen
Email: [email protected]
Tel: +45 65502439.
Bisphenol A (BPA) at Very Low Levels Can Adversely Affect Developing Organs in Primates, MU Researcher Finds

|
Bisphenol A (BPA) is a chemical that is used in a wide variety of consumer products, such as resins used to line metal food and beverage containers, thermal paper store receipts, and dental composites. BPA exhibits hormone-like properties, and exposure of fetuses, infants, children or adults to the chemical has been shown to cause numerous abnormalities, including cancer, as well as reproductive, immune and brain-behavior problems in rodents. Now, researchers at the University of Missouri have determined that daily exposure to very low concentrations of BPA by pregnant females also can cause fetal abnormalities in primates.
“BPA is an endocrine disrupting chemical that has been demonstrated to alter signaling mechanisms involving estrogen, androgen and thyroid hormones,” said Frederick vom Saal, Curators Professor of Biological Sciences in the College of Arts and Science at MU. “Previous studies in rodents have demonstrated that maternal exposure to very low doses of BPA can significantly alter fetal development, resulting in a variety of adverse outcomes in the fetus. Our study is one of the first to show this also happens in primates.”
Although BPA is considered a toxic chemical in other countries such as Canada, the U.S. has been slow to address the issue, said vom Saal. Until now, most studies involving BPA have been conducted on laboratory mice and rats, leading U.S. regulatory agencies to call for studies in primates. With funding provided by the National Institute of Environmental Health Sciences (NIEHS), a research institute of the National Institutes of Health, vom Saal and his colleagues studied the chemical’s blood levels in pregnant female rhesus monkeys and their fetuses, which are considered to be very similar to human fetuses.
After collecting tissue samples, other researchers analyzed the tissues to determine if BPA exposure was harmful to fetal development. Researchers found evidence of significant adverse effects in mammary glands, ovaries, brain, uterus, lung and heart tissues in BPA exposed fetus when compared to fetuses not exposed to BPA. The abnormalities were caused by levels of BPA in the monkey fetuses that were very similar to levels reported in previous studies of BPA in human fetuses.
“The very low-level exposure to BPA we delivered once a day to the rhesus monkeys is far less than the BPA levels humans are exposed to each day, which reflects multiple exposures,” vom Saal said. “Our findings suggest that traditional toxicological studies likely underestimate actual human exposure and show, unequivocally, that biologically active BPA passes from the mother to the fetus. Additionally, our latest study shows that BPA causes damage to developing systems of monkey fetuses, and this is of great concern for human fetuses.”
The study, “Bisphenol A (BPA) pharmacokinetics with daily oral bolus or continuous exposure via silastic capsules in pregnant rhesus monkeys: relevance for human exposures,” was funded in part by the NIEHS and was published in Reproductive Toxicology in collaboration with Catherine A. VandeVoort with the Department of Obstetrics and Gynecology and the California National Primate Research Center at the University of California, Davis; Julia A. Taylor and Wade V. Welshons with the University of Missouri; Pierre-Louis Toutain with the Univesite de Toulouse; and Patricia A Hunt with the School of Molecular Biosciences at Washington State University.
###
Published by the MU News Bureau
Study Reveals Evolution at Work

|
New research by UC Santa Barbara’s Kenneth S. Kosik, Harriman Professor of Neuroscience, reveals some very unique evolutionary innovations in the primate brain.
In a study published online today in the journal Neuron, Kosik and colleagues describe the role of microRNAs - so named because they contain only 22 nucleotides - in a portion of the brain called the outer subventricular zone (OSVZ). These microRNAs belong to a special category of noncoding genes, which prevent the formation of proteins.
“It’s microRNAs that provide the wiring diagram, dictating which genes are turned on, when they’re turned on and where they’re turned on,” said Kosik, who is also the co-director of UCSB’s Neuroscience Research Institute and a professor in the Department of Molecular, Cellular and Developmental Biology. “There’s a core set with which all kinds of really complex things can be built, and these noncoding genes know how to put it together.”
The researchers were looking for these noncoding genes, Kosik continued, because as organisms become more complex through evolution, the number of these noncoding genes has greatly expanded. “But the coding genes - the ones that make proteins - have really not changed very much,” he said. “The action has been in this noncoding area and what that part of the genome is doing is controlling the genes.”
Many of the microRNAs that Kosik’s team found and subsequently sequenced are newly evolved in primates. The work showed that these tiny control elements were overrepresented in the OSVZ of the developing macaque brain tissues they analyzed. The tissue samples were provided by a lab at the Stem-cell and Brain Research Institute near Lyon, France, headed by research director and co-author Colette Dehay.
Study results indicate that the appearance of the OSVZ is very much associated with the invention of new microRNAs. “There might be some relationship - although we can’t prove it - between the invention of some of these new noncoding genes, microRNAs, and the appearance of a new structure, the OSVZ,” Kosik said. “Trying to connect an anatomical, morphological invention with genes is very difficult, but our work shows a possible molecular basis for the tools that were needed to build this novel structure.”
The analysis found that these new microRNAs target old genes, many involved in the cell cycle, which is responsible for cell division (mitosis). “Nearly all cells throughout evolution have a cell cycle,” Kosik explained. “We can watch the evolutionary process at a very molecular level, see what is novel and how molecular innovation affects what already exists, like the cell cycle. When new things are invented in evolution, they have to be integrated with what already exists.
“What I find fascinating is that the whole ancient cellular mechanism of cell division still has enough evolutionary space left to make something new and to make something new that’s really complex,” he added. “The OSVZ gave rise to primates’ expanded brains and to the cells that ultimately brought us Shakespeare.”
According to Kosik, the microRNAs he studied are a melding of molecular and anatomical information. “Some of the genes we found that are the targets of these new microRNAs are also involved in certain human developmental disorders that are genetic,” he said.
“One place we would like to go with this information is to explore pathways that may be manipulated to help patients in some way,” he said. “We know people with developmental disorders may be missing a critical gene involved in brain formation and wiring, so maybe if we understood the control of those genes - as these new data are pointing to - we might be able to do something that could be applied to a human condition.”
Contact Info:
Julie Cohen
[email protected]
(805) 893-7220
Print Version
Tell-a-Friend comments powered by Disqus
| RELATED ARTICLES: |





